Abstract
The airways and the urinary bladder are both hollow organs serving very different functions, i.e. air flow and urine storage, respectively. While the autonomic nervous system seems to play only a minor if any role in the physiological regulation of airway tone during normal breathing, it is important in the physiological regulation of bladder smooth muscle contraction and relaxation. While both tissues share a greater expression of M2 than of M3 muscarinic receptors, smooth muscle contraction in both is largely mediated by the smaller M3 population apparently involving phospholipase C activation to only a minor if any extent. While smooth muscle in both tissues can be relaxed by β-adrenoceptor stimulation, this primarily involves β 2-adrenoceptors in human airways and β 3-adrenoceptors in human bladder. Despite activation of adenylyl cyclase by either subtype, cyclic adenosine monophosphate plays only a minor role in bladder relaxation by β-agonists; an important but not exclusive function is known in airway relaxation. While airway β 2-adrenoceptors are sensitive to agonist-induced desensitization, β 3-adrenoceptors are generally considered to exhibit much less if any sensitivity to desensitization. Gene polymorphisms exist in the genes of both β 2- and β 3-adrenoceptors. Despite being not fully conclusive, the available data suggest some role of β 2-adrenoceptor polymorphisms in airway function and its treatment by receptor agonists, whereas the available data on β 3-adrenoceptor polymorphisms and bladder function are too limited to allow robust interpretation. We conclude that the distinct functions of airways and urinary bladder are reflected in a differential regulation by the autonomic nervous system. Studying these differences may be informative for a better understanding of each tissue.
Similar content being viewed by others
The airways and the urinary bladder are hollow organs. Their walls contain smooth muscle which allows for contraction and relaxation. The inner surface of both is covered by an epithelial layer, which is termed urothelium in the bladder and respiratory epithelium in the airways. The function of both organs is primarily regulated by the autonomic nervous system, but bladder contraction to a certain degree is under voluntary control. However, the airways and the bladder serve very different purposes within the mammalian body. While the airways are filled with air and primarily serve the purpose of air flow to ultimately yield gas exchange, the bladder is filled with urine and allows for only limited absorption and secretion (Krege et al. 2004). While the airways undergo several filling/emptying cycles every minute, only one such cycle occurs in a healthy human bladder every couple of hours. This article will explore how the autonomic control of smooth muscle function differs between the airways and the bladder. A general summary of key features is presented in Table 1.
Physiological considerations
Filling of both the airways and the bladder is primarily driven by forces outside the tissue. In the case of the airways, filling during inhalation occurs largely passively as a result of the contraction of striated muscles such as the diaphragm which increases intrathoracic volume. The relaxation of airway smooth muscle serves only a modulating role in accommodating the air, as it is used to lower airway resistance under conditions of physical or emotional stress when the organisms needs extra oxygen. Thus, even a maximum relaxation of airway smooth muscle increases airway volume by much less than 100%. This airway smooth muscle relaxation is mediated by β-adrenoceptors, largely belonging to the β 2 subtype in several mammalian species including humans (Mak et al. 1996). The bladder filling is also largely driven passively as it occurs secondary to the urine output by the kidneys. However, the relaxation of bladder smooth muscle plays a crucial role in this process as it allows accommodating increasing volumes of urine without major increases in intravesical pressure (Andersson 1993). Considering that the physiological amount of urine in the bladder at the start of each micturition cycle is less than 50 ml and that a healthy bladder can easily hold 500 ml of urine, the bladder must accommodate greater than tenfold changes in volume and hence have an enormous compliance. This compliance is mainly mediated by β-adrenoceptor-driven bladder smooth muscle relaxation, which in most mammalian species including humans predominantly occurs via the β 3 subtype (Michel and Vrydag 2006).
Emptying of the lung is largely driven by its elastic properties. The autonomic nervous system does not play a major role in narrowing airway diameter during physiological breathing; however, it can cause major airway contraction as a defense against inhaled toxic substances or during pathophysiological conditions. Paradoxically, instead of improving emptying, parasympathetically evoked bronchial smooth muscle contraction impairs it by increasing airway resistance. Such contraction is mediated by muscarinic acetylcholine receptors of the M3 subtype (Fisher et al. 2004). In contrast, the physiological emptying of the urinary bladder is largely mediated by bladder smooth muscle contraction. Nevertheless, this process is also driven by muscarinic receptors of the M3 subtype (Hegde 2006). While bladder emptying is driven by smooth muscle contraction in the detrusor, it is accompanied by muscle relaxation of the urethra to allow an undisturbed flow of urine. However, the autonomic control of the urethra will not be discussed here. Interestingly, the major difference in the length of a filling/emptying cycle between airways and bladder (seconds vs. hours) is largely due to differences in the length of the filling phase, whereas the emptying phase occurs almost equally quickly in both tissues. It is tempting to speculate that the differential role of β 2- vs. β 3-adrenoceptors in relaxation as compared to the similar role of M3 receptors in contraction may relate to these differences in the duration of filling. The following will discuss in more detail similarities and differences in the regulation of airway and bladder smooth muscle contraction and relaxation by muscarinic receptors and β-adrenoceptors, respectively.
Parasympathetic control of smooth muscle contraction
While the parasympathetic innervation of the airways is provided by the vagus nerve, that of the bladder comes from the pelvic nerves originating in the sacral spinal cord. However, in both tissues the acetylcholine may also come from non-neuronal sources (see below). Smooth muscle from both tissues expresses mainly the M2 and the M3 subtype of muscarinic receptors, and in many species the M2 subtype is expressed more prominently than the M3 subtype at both the mRNA and the protein level (Coulson and Fryer 2003; Goepel et al. 1998; Roffel et al. 1988). Nevertheless, smooth muscle contraction of the airways (Coulson and Fryer 2003; Roffel et al. 1990, 1988) and the bladder (Abrams et al. 2006; Hegde 2006) occurs largely if not exclusively by M3 receptors. Accordingly, isolated airway tissue from M2 receptor knock-out mice shows only modest impairment of muscarinic agonist-induced contraction (Stengel et al. 2000; Struckmann et al. 2003) or bladder contractility (Igawa et al. 2004), whereas M3 receptor knock-out mice exhibit major impairments in both tissues (Fisher et al. 2004; Igawa et al. 2004; Matsui et al. 2000; Stengel et al. 2002; Struckmann et al. 2003). Accordingly, antagonists which preferentially inhibit M3 receptors such as tiotropium (Disse et al. 1999; Koumis and Samuel 2005) in the airways and darifenacin (Croom and Keating 2004; Maruyama et al. 2006) and solifenacin (Armstrong et al. 2008; Chapple 2006; Oki et al. 2005) in the bladder appear to have similar therapeutic efficacy as non-selective muscarinic antagonists, further supporting the major role of M3 receptors in regulating contraction in both tissues. However, in both airways and bladder M2 receptors may have a physiological role in opposing smooth muscle relaxation mediated by β-adrenoceptors during the filling phase (Ehlert et al. 2007; Matsui et al. 2003; Sarria et al. 2002). Moreover, at least in airways, prejunctional inhibitory M2 receptors play a major role in regulating smooth muscle tone (Coulson and Fryer 2003). While prejunctional muscarinic receptors also exist in the bladder, they appear to play a smaller functional role in the regulation of smooth muscle tone than those in the airways. Nevertheless, prejunctional inhibitory M2-receptors also exist in the bladder (Trendelenburg et al. 2003) but additional inhibitory M4-receptors (D'Agostino et al. 1997, 2000) and facilitatory M1-receptors also exist (Somogyi et al. 1996).
A stimulation of phospholipase C (PLC) with the subsequent formation of inositoltrisphosphate and diacylglycerol is the prototypical signalling pathway of M3 receptors. This can also be shown in airways (An and Hai 1999) and bladder (Kories et al. 2003) using subtype-selective antagonists, and studies with knock-out mice confirm such observations (Tran et al. 2006). Nevertheless, PLC does not appear to contribute to bladder contraction by muscarinic agonists in a major way. This was first proposed based upon the PLC inhibitor U 73,122 in rat (Schneider et al. 2004b), mouse (Wegener et al. 2004) and human bladder (Schneider et al. 2004a); in those studies U 73,122 did not affect bladder contraction in concentrations where it fully suppressed inositol phosphate formation (Schneider et al. 2004b). However, using different experimental designs and different PLC inhibitors other investigators have proposed a role for PLC in bladder contraction (Braverman et al. 2006a, b). In a subsequent collaborative study between the groups reporting evidence in favor and against a role for PLC in bladder contraction, it was found that previously shown differences relate to the choice of PLC inhibitor rather than experimental conditions; more importantly, the overall evidence did not support a major role of PLC in bladder contraction (Frazier et al. 2007). Thus, despite a prominent role for PLC in M3 receptor function, other signalling pathways apparently carry M3 muscarinic receptor-mediated contraction bladder contraction (Frazier et al. 2008). Interestingly, some muscarinic receptor antagonists such as propiverine and its metabolites also have direct effects on Ca2 influx, which may contribute to their clinical effects (Wuest et al. 2006, 2007). While we are not aware of similar systematic studies in the airways, it has been shown that Ca2 oscillations in the airways do not necessarily require PLC activation (Sney et al. 2003). Similar to the bladder, other signalling pathways including cyclic ADP-ribose and Rho-kinase may be relevant for muscarinic receptor-mediated airway contraction (Deshpande et al. 2005; Lutz et al. 2005).
While the classical view dictated that formation of neurotransmitters is an exclusive property of neurons, it has meanwhile become clear that non-neuronal acetylcholine formation exists in several tissues. Major parts of the evidence in this regard come from the airways, the intestine, the skin, and the urinary bladder. Thus, the urothelium expresses the enzymes required for acetylcholine synthesis and forms acetylcholine (Lips et al. 2007). Urothelium-derived acetylcholine may act on muscarinic receptors within the urothelium including those on afferent sensory nerves as well as those on bladder smooth muscle (Bschleipfer et al. 2007; Zarghooni et al. 2007). Airways smooth muscle, goblet, basal, mast, and ciliated cells also express choline acetyl transferase and/or produce acetylcholine, and this has been proposed to be a potential target of drug treatment (Wessler and Kirkpatrick 2001).
Sympathetic control of smooth muscle relaxation
While all three classes of adrenoceptors are expressed in both airways and bladder, postjunctional α1- and α2-adrenoceptors do not contribute to the regulation of smooth muscle tone in either tissue in a major way (Goldie et al. 1990; Michel and Vrydag 2006). While β-adrenoceptors are abundantly expressed in both tissues, they mostly belong to the β 2-subtype in the airways of many mammalian species including humans (Goldie et al. 1990). The expression pattern of β-adrenoceptor subtypes in the bladder is less clear. In humans, the β 3-subtype appears to be by far the most prominently expressed subtype at the mRNA level (Nomiya and Yamaguchi 2003; Otsuka et al. 2008). Quantitative data on mRNA expression of β-adrenoceptor subtypes in other species are not available. Data on protein expression of β-adrenoceptor subtype expression in the bladder are not conclusive as no validated antibodies or suitable radioligands exist (Niclauß et al. 2006; Vrydag and Michel 2007).
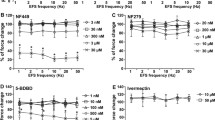
Functional studies demonstrate very clearly that the β-adrenoceptor-mediating airway smooth muscle relaxation belongs predominantly if not exclusively to the β 2-subtype (Goldie et al. 1990) although in some species, e.g. guinea pigs, β 1-adrenoceptors may contribute (Tanaka et al. 2007). In most species β 3-adrenoceptors make a substantial contribution to bladder relaxation and may be the only subtype of functional relevance in the human bladder (Michel and Vrydag 2006). Thus, airways and bladder differ considerably with regard to the β-adrenoceptor subtypes being expressed and mediating smooth muscle relaxation.
The prototypical signalling pathway of β-adrenoceptors is a Gs-mediated coupling to an activation of adenylyl cyclase leading to the formation of cyclic adenosine monophosphate (cAMP). However, data from various cell types indicate that other signalling pathways may also be functionally relevant (Scherer et al. 2007) and, e.g. in vascular smooth muscle the activation of certain types of K channels is a major pathway involved in β-adrenoceptor-mediated relaxation (Bieger et al. 2006; Ferro 2006). Other signalling pathways such as cyclooxygenase (Kang et al. 2007) or NO synthase (Bieger et al. 2006) may also be involved. Against this background, several studies have evaluated the contribution of the cAMP/protein kinase A pathway relative to other signalling pathways in the β-adrenoceptor-mediated relaxation of airway and bladder smooth muscle. In the urinary bladder, two independent studies in rats demonstrate that cAMP formation plays only a minor if any role in smooth muscle relaxation whereas K channels, particularly of the BKCa type may make major contributions (Frazier et al. 2005; Uchida et al. 2005). Similar studies in the airways of various species including humans (Miura et al. 1992) have also indicated major cAMP-independent components of relaxation responses to β-adrenoceptor stimulation, including the stimulation of BKCa channels (Giembycz and Newton 2006; Johnson 2006).
β 2-Adrenoceptors are known to undergo a rapid and profound agonist-induced desensitization which under chronic conditions involves down-regulation of the receptor (Tran et al. 2007). Accordingly, β 2-adrenoceptors in the lung have also been shown to undergo agonist-induced desensitization (Finney et al. 2001; Hauck et al. 1997; January et al. 1998). This may become therapeutically important during chronic treatment with β-adrenergic agonists, but its clinical importance remains controversial (Johnson 2006). In contrast, β 3-adrenoceptors lack the phosphorylation sites believed to be important in desensitization and are believed to be relatively resistant to agonist-induced desensitization (Carpene et al. 1993; Chaudhry and Granneman 1994). Preliminary data indicate that rat bladder β-adrenoceptors may undergo some agonist-induced desensitization but it remains to be determined if that affects the β 3-component of the response (Vrydag and Michel 2008). A possible rationale for this difference between airways and bladder may be rooted in the fact that the bladder β-adrenoceptors have to function during a filling phase of several hours, which would be hampered if they undergo rapid desensitization. However, detailed studies on the sensitivity of bladder β-adrenoceptors in response to prolonged agonist exposure have not been reported.
The regulation of lung and bladder β-adrenoceptors has also been studied during ageing and in pathophysiological settings. Airway β 2-adrenoceptor function may be reduced in aged animals (Fraeyman et al. 1993; Preuss et al. 1999), and a minor desensitization of bladder β-adrenoceptors has also been reported in aged rats (Michel and Barendrecht 2008). In contrast to e.g. cardiac β 1-adrenoceptors, the β 2-adrenoceptors in the lung do not exhibit down-regulation in spontaneously hypertensive rats but rather may even be up-regulated (Michel et al. 1987) and functionally have enhanced sensitivity to agonist stimulation (Kamibayashi and Ramanathan 1989). In contrast, β-adrenoceptors in the bladder of spontaneously hypertensive rats were reported to exhibit a minor desensitization (Frazier et al. 2006).
Within the bladder, β-adrenoceptors are not only expressed on smooth muscle cells but also on the urothelium (Harmon et al. 2005). Their stimulation may affect the ability of β-adrenoceptor agonists to induce bladder relaxation (Otsuka et al. 2008). Similarly, airway β-adrenoceptors are also not only found on smooth muscle but also on ciliated epithelial and mucus cells, where they can increase the beating frequency of the cilia and discharge of glycoprotein, respectively; moreover, β 2-adrenoceptors on lung mast cells may indirectly affect lung function by inhibiting the release of the bronchoconstrictor histamine (Johnson 2006; Johnson and Rennard 2001).
The genes of all three β-adrenoceptor subtypes are polymorphic (Leineweber et al. 2004). Studies with regard to pulmonary function have focused on polymorphisms in the amino acid positions 16 and 49 of the β 2-adrenoceptor and indicate that such polymorphisms may affect the speed of agonist-induced desensitization of airway smooth muscle cells (Moore et al. 2000) and also on lung mast cells (Chong et al. 2000; Kay et al. 2003). Whether this translates into clinically relevant effects on the prevalence of airways disease or its treatment by β-adrenoceptor agonists, remains controversial (Brodde and Leineweber 2005; Szalai et al. 2008; Thakkinstian et al. 2005). β 2-Adrenoceptor polymorphisms may also play a role as modifying-genes in diseases such as cystic fibrosis (Büscher and Grasemann 2006). With regard to β 3-adrenoceptor polymorphisms and bladder function, only a single study has been reported until now demonstrating that the Trp64Arg polymorphism is more frequently present in patients with overactive bladder syndrome than in those without (Honda et al. 2006).
β 2-Adrenoceptor agonists have long been used as bronchodilating drugs, whereas only very recently a single proof-of-concept study has demonstrated that a β 3-adrenoceptor agonist may alleviate bladder dysfunction in patients with overactive bladder (Chapple et al. 2008). However, the chronic use of β 2-adrenoceptor agonists in the treatment of airway disease has been questioned on safety grounds (Salpeter et al. 2006). In contrast, it has been reported that chronic (but not acute) administration of β-adrenoceptor antagonists may have beneficial effects in mouse models of asthma (Callaerts-Vegh et al. 2004; Nguyen et al. 2008). Therefore, in analogy to the situation in heart failure (Brodde 2007), it has been advocated that β-adrenoceptor antagonists may have some value in the chronic treatment of asthma (Bond et al. 2007). A clinical pilot study in asthma patients has been reported which supports such claims (Hanania et al. 2008). The relative benefits of agonist and antagonist treatment in airway and bladder disease certainly requires considerable additional study.
Conclusions
Based upon their differential functions, the morphology and autonomic control differs considerably between the airways and the urinary bladder. Nevertheless, a number of interesting similarities exist in the way the autonomic system controls the two tissues. Moreover, the differences in autonomic control may also be quite informative, particularly with regard to the relative role of β-adrenoceptor subtypes. Therefore, we propose that researchers interested in the autonomic control of either tissue may benefit from keeping an eye on the other tissue. While beyond the scope of this article, expanding the scope even further to other hollow organs including the gut and the heart (Brodde and Michel 1999) may provide additional comparative insight.
References
Abrams P, Andersson K-E, Buccafusco JJ, Chapple C, De Groat WC, Fryer AD, Kay G, Laties A, Nathanson NM, Pasricha PJ, Wein AJ (2006) Muscarinic receptors: their distribution and function in body systems, and the implications for treating overactive bladder. Br J Pharmacol 148:565–578
An SS, Hai CM (1999) Mechanical strain modulates maximal phosphatidylinositol turnover in airway smooth muscle. Am J Physiol 277:L968–L974
Andersson K-E (1993) Pharmacology of lower urinary tract smooth muscles and penile erectile tissues. Pharmacol Rev 45:253–308
Armstrong SR, Briones S, Horger B, Richardson CL, Jaw-Tasi S, Hegd SS (2008) Pharmacological analysis of the interaction of antimuscarinic drugs at M2 and M3 muscarinic receptors in vivo using the pithed rat assay. Naunyn-Schmiedeberg's Arch Pharmacol 376:341–349
Bieger D, Parai K, Ford CA, Tabrizchi R (2006) β-Adrenoceptor mediated responses in rat pulmonary artery: putative role of TASK-1 related K channels. Naunyn-Schmiedeberg's Arch Pharmacol 373:186–196
Bond RA, Spina D, Parra S, Page CP (2007) Getting to the heart of asthma: can “β blockers” be useful to treat asthma? Pharmacol Ther 115:360–374
Braverman AS, Doumanian LR, Ruggieri MR Sr (2006a) M2 and M3 muscarinic receptor activation of urinary bladder contractile signal transduction. II. Denervated rat bladder. J Pharmacol Exp Ther 316:875–880
Braverman AS, Tibb AS, Ruggieri MR Sr (2006b) M2 and M3 muscarinic receptor activation of urinary bladder contractile signal transduction. I. Normal rat bladder. J Pharmacol Exp Ther 316:869–874
Brodde O-E (2007) β-Adrenoceptor blocker treatment and the cardiac β-adrenoceptor-G-protein(s)-adenylyl cyclase system in chronic heart failure. Naunyn-Schmiedeberg's Arch Pharmacol 374:361–372
Brodde O-E, Leineweber K (2005) β2-Adrenoceptor gene polymorphisms. Pharmacogenetics and Genomics 15:267–275
Brodde O-E, Michel MC (1999) Adrenergic and muscarinic receptors in the human heart. Pharmacol Rev 51:651–689
Bschleipfer T, Schukowski K, Weidner W, Grando SA, Schwantes U, Kummer W, Lips KS (2007) Expression and distribution of cholinergic receptors in the human urothelium. Life Sci 80:2303–2307
Büscher R, Grasemann H (2006) Disease modifying genes in cystic fibrosis: therapeutic option or one-way road? Naunyn-Schmiedeberg's Arch Pharmacol 374:65–77
Callaerts-Vegh Z, Evans KLJ, Dudekula N, Cuba D, Knoll BJ, Callaerts PFK, Giles H, Shardonofsky FR, Bond RA (2004) Effects of acute and chronic administration of β-adrenoceptor ligands on airway function in a murine model of asthma. Proc Natl Acad Sci USA 101:4948–4953
Carpene C, Galitzky J, Collon P, Esclapez F, Dauzats M, Lafontan M (1993) Desensitization of beta-1 and beta-2, but not beta-3 adrenoceptor-mediated lipolytic responses of adipocytes after long-term norepinephrine infusion. J Pharmacol Exp Ther 265:237–247
Chapple CR (2006) Solifenacin provides effective antimuscarinic therapy for the complete management of overactive bladder. Exp Opin Pharmacother 7:2421–2434
Chapple CR, Yamaguchi O, Ridder A, Liehne J, Carl S, Mattiasson A, Aramburu MAL, Lucas M, Everaert K (2008) Clinical proof of concept study (Blossom) shows novel β3 adrenoceptor agonist YM178 is effective and well tolerated in the treatment of symptoms of overactive bladder. Eur Urol Suppl 7:239
Chaudhry A, Granneman JG (1994) Influence of cell type upon the desensitization of the β3-adrenergic receptor. J Pharmacol Exp Ther 271:1253–1258
Chong LK, Chowdry J, Ghahramani P, Peachell PT (2000) Influence of genetic polymorphisms in the β2-adrenoceptor on desensitisation in human lung mast cells. Pharmacogenetics 10:153–162
Coulson FR, Fryer AD (2003) Muscarinic acetylcholine receptors and airway diseases. Pharmacol Ther 98:59–69
Croom KF, Keating GM (2004) Darifenacin in the treatment of overactive bladder. Drugs Aging 21:885–892
D’Agostino G, Barbieri A, Chiossa E, Tonini M (1997) M4 muscarinic autoreceptor-mediated inhibition of [3H]acetylcholine release in the rat isolated urinary bladder. J Pharmacol Exp Ther 283:750–756
D’Agostino G, Bolognesi ML, Lucchelli A, Vicini D, Balestra B, Spelta V, Melchiorre C, Tonini M (2000) Prejunctional muscarinic inhibitory control of acetylcholine release in the human isolated detruso: involvement of the M4 receptor subtype. Br J Pharmacol 129:493–500
Deshpande DA, White TA, Dogan S, Walseth TF, Panettieri RA, Kannan MS (2005) CD38/cyclic ADP-ribose signaling: role in the regulation of calcium homeostasis in airway smooth muscle. Am J Physiol 288:L773–L788
Disse B, Speck GA, Rominger KL, Witek TJ Jr, Hammer R (1999) Tiotropium (Spiriva): mechanistical considerations and clinical profile in obstructive lung disease. Life Sci 64:456–464
Ehlert FJ, Ahn S, Pak KJ, Park GJ, Sangnil MS, Tran JA, Matsui M (2007) Neuronally release acetylcholine acts on the M2 muscariic receptor to oppose the relaxant effect of isoproterenol on cholinergic contractions in mouse urinary bladder. J Pharmacol Exp Ther 322:631–637
Ferro A (2006) β-Adrenoceptors and potassium channels. Naunyn-Schmiedeberg's Arch Pharmacol 373:183–185
Finney PA, Donnelly LE, Belvisi MG, Chuang T-T, Birrell M, Harris A, Mak JCW, Scorer C, Barnes PJ, Adcock IM, Giembycz MA (2001) Chronic systemic administration of salmeterol to rats promotes pulmonary β2-adrenoceptor desensitization and down-regulation of Gsa. Br J Pharmacol 132:1261–1270
Fisher JT, Vincent SG, Gomeza J, Yamada M, Wess J (2004) Loss of vagally mediated bradycardia and bronchoconstriction in mice lacking M2 or M3 muscarinic acetylcholine receptors. FASEB J 18:711–713
Fraeyman N, Vanscheeuwijck P, de Wolf M, Quatacker J (1993) Influence of aging on fluidity and coupling between β-receptors and G-proteins in rat lung membranes. Life Sci 53:153–160
Frazier EP, Mathy M-J, Peters SLM, Michel MC (2005) Does cyclic AMP mediate rat urinary bladder relaxation by isoproterenol? J Pharmacol Exp Ther 313:260–267
Frazier EP, Schneider T, Michel MC (2006) Effects of gender, age and hypertension on b-adrenergic receptor function in rat urinary bladder. Naunyn-Schmiedeberg's Arch Pharmacol 373:300–309
Frazier EP, Braverman AS, Peters SLM, Michel MC, Ruggieri MR Sr (2007) Does phospholipase C mediate muscarinic receptor-induced rat urinary bladder contraction? J Pharmacol Exp Ther 322:998–1002
Frazier EP, Peters SLM, Braverman AS, Ruggieri MR Sr, Michel MC (2008) Signal transduction underlying control of urinary bladder smooth muscle tone by muscarinic receptors and b-adrenoceptors. Naunyn-Schmiedeberg's Arch Pharmacol 377:449–462
Giembycz MA, Newton R (2006) Beyond the dogma: novel β2-adrenoceptor signalling in the airways. Eur Resp J 27:1286–1306
Goepel M, Gronewald A, Krege S, Michel MC (1998) Muscarinic receptor subtypes in porcine detrusor: comparison with humans and regulation by bladder augmentation. Urol Res 26:149–154
Goldie RG, Paterson JW, Lulich KM (1990) Adrenoceptors in airway smooth muscle. Pharmacol Ther 48:295–322
Hanania NA, Singh S, El-Wali R, Flashner M, Franklin AE, Garner WJ, Dickey BF, Parra S, Ruoss S, Shardonofsky FR, OÇonnor BJ, Page C, Bond RA (2008) The safety and effects of the beta-blocker, nadolol, in mild asthma: an open-label pilot study. Pulm Pharmacol Ther 21:134–141
Harmon EB, Porter JM, Porter JE (2005) β-Adrenergic receptor activation in immortalized human urothelial cells stimulates inflammatory responses by PKD-independent mechanisms. Cell Commun Signal 3:10
Hauck RW, Harth M, Schulz C, Präuer H, Böhm M, Schömig A (1997) Effects of β2-agonist- and dexamethasone-treatment on relaxation and regulation of β-adrenoceptors in human bronchi and lung tissue. Br J Pharmacol 121:1523–1530
Hegde SS (2006) Muscarinic receptors in the bladder: from basic research to therapeutics. Br J Pharmacol 147:S80–S87
Honda K, Nomiya M, Shishido K, Yoshimura Y, Yamaguchi O (2006) Mutation of β3-adrenoceptor gene: a genetic marker for overactive bladder. Neurourol Urodyn 25:652
Igawa Y, Zhang X, Nishizawa O, Umeda M, Iwata A, TAketo MM, Manabe T, Matsui M, Andersson K-E (2004) Cystometric findings in mice lacking muscarinic M2 or M3 receptors. J Urol 172:2460–2464
January B, Seibold A, Allal C, Whaley BS, Knoll BJ, Moore RH, Dickey BF, Barber R, Clark RB (1998) Salmeterol-induced desensitization, internalization and phosphorylation of the human β2-adrenoceptor. Br J Pharmacol 123:701–711
Johnson M (2006) Molecular mechanisms of β2-adrenergic receptor function, response, and regulation. J Allergy Clin Immunol 117:18–24
Johnson M, Rennard S (2001) Alternative mechanisms for long-acting β2-adrenergic agonists in COPD. Chest 120:258–270
Kamibayashi C, Ramanathan S (1989) Supersensitivity of beta-adrenoceptor coupled adenylate cyclase in pulmonary tissue of the spontaneously hypertensive rat. Life Sci 45:2115–2125
Kang KB, Rajanayagam MAS, van der Zypp A, Majewski H (2007) A role for cyclooxygenase in aging-related changes of β-adrenoceptor-mediated relaxation in rat aortas. Naunyn-Schmiedeberg's Arch Pharmacol 375:273–281
Kay LJ, Chong LK, Rostami-Hodjegan A, Peachell PT (2003) Influence of the thr164ile polymorphism in the β2-adrenoceptor on the effects of b-adrenoceptor agonists on human lung mast cells. Int Immunopharmacol 3:91–95
Kories C, Czyborra C, Fetscher C, Schneider T, Krege S, Michel MC (2003) Gender comparison of muscarinic receptor expression and function in rat and human urinary bladder: differential regulation of M2 and M3? Naunyn-Schmiedeberg's Arch Pharmacol 367:524–531
Koumis T, Samuel S (2005) Tiotropium bromide: a new long-acting bronchodilator for the treatment of chronic obstructive pulmonary disease. Clin Ther 27:377–392
Krege S, Kinzig-Schppers M, Sörgel F, Baschek R, Michel MC, Rübben H (2004) Absorption of intravesically applied drugs: comparison of normal and ileal-augmented rabbit bladder. J Urol 172:2045–2050
Leineweber K, Büscher R, Bruck H, Brodde O-E (2004) β-Adrenoceptor polymorphisms. Naunyn-Schmiedeberg's Arch Pharmacol 369:1–22
Lips KS, Wunsch J, Sarghooni S, Bschleipfer T, Schukowski K, Weidner W, Wessler I, Schwantes U, Koepsell H, Kummer W (2007) Acetylcholine and molecular components of its synthesis and release machinery in the urothelium. Eur Urol 51:1042–1053
Lutz S, Freichel-Blomquist A, Yang Y, Rümenapp U, Jakobs K-H, Schmidt M, Wieland T (2005) The guanine nucleotide exchange factor p63RhoGEF, a specific link between Gq/11-coupled receptor signaling and RhoA. J Biol Chem 280:11134–11139
Mak JCW, Nishikawa M, Haddad E-B, Kwon O-J, Hirst SJ, Twort CHC, Barnes PJ (1996) Localisation and expression of β-adrenoceptor subtype mRNAs in human lung. Eur J Pharmacol 302:215–221
Maruyama S, Oki T, Otsuka A, Shinbo H, Ozono S, Kageyama S, Mikami Y, Araki I, Takeda M, Masuyama K, Yamada S (2006) Human muscarinic receptor binding characteristics of antimuscarinic agents to treat overactive bladder. J Urol 175:365–369
Matsui M, Motomura D, Karasawa H, Fujikawa T, Jiang J, Komiya Y, Takahashi S, TAketo MM (2000) Multiple functional defects in peripheral autonomic organs in mice lacking muscarinic acetylcholine receptor gene for the M3 subtype. Proc Natl Acad Sci USA 97:9579–9584
Matsui M, Griffin MT, Shehnaz D, TAketo MM, Ehlert FJ (2003) Increased relaxant action of forskolin and isoproterenol against muscarinic agonist-induced contractions in smooth muscle from M2 receptor knockout mice. J Pharmacol Exp Ther 305:106–113
Michel MC, Barendrecht MM (2008) Physiological and pathological regulation of the autonomic control of urinary bladder contractility. Pharmacol Ther 117:297–312
Michel MC, Vrydag W (2006) α1-, α2- and β-adrenoceptors in the urinary bladder, urethra and prostate. Br J Pharmacol 147:S88–S119
Michel MC, Wang XL, Schlicker E, Göthert M, Beckeringh JJ, Brodde O-E (1987) Increased β2-adrenoceptor density in heart, lung and kidney of spontaneously hypertensive rats. J Auton Pharmacol 7:41–51
Miura M, Belvisi MG, Stretton CD, Yacoub MH, Barnes PJ (1992) Role of potassium channels in bronchodilator responses in human airways. Am Rev Respir Dis 146:132–136
Moore PE, Laporte JD, Abraham JH, Schwartzman IN, Yandava CN, Silverman ES, Drazen JM, Wand MP, Panettieri RA, Shore SA (2000) Polymorphism of the β2-adrenergic receptor gene and desensitization in human airways smooth muscle. Am J Respir Crit Care Med 162:2117–2124
Nguyen LP, Omoluabi O, Parra S, Frieske JM, Clement C, Ammar-Auchiche Z, Ho SB, Ehre C, Kesimer M, Knoll BJ, Tuvim MJ, Dickey BF, Bond RA (2008) Chronic exposure to beta-blockers attenuates inflammation and mucin content in a murine asthma model. Am J Respir Cell Mol Biol 38:256–262
Niclauβ N, Michel-Reher MB, Alewijnse AE, Michel MC (2006) Comparison of three radioligands for the labelling of human β-adrenoceptor subtypes. Naunyn-Schmiedeberg's Arch Pharmacol 374:79–85
Nomiya M, Yamaguchi O (2003) A quantitative analysis of mRNA expression of α1 and β-adrenoceptor subtypes and their functional roles in human normal and obstructed bladders. J Urol 170:649–653
Oki T, Sato S, Miyata K, Yamada S (2005) Muscarinic receptor binding, plasma concentration and inhibition of salivation after oral administration of a novel antimuscarinic agent, solifenacin succinate in mice. Br J Pharmacol 145:219–227
Otsuka A, Shinbo H, Matsumoto R, Kurita Y, Ozono S (2008) Expression and functional role of β-adrenoceptors in the human urinary bladder. Naunyn-Schmiedeberg's Arch Pharmacol 377:473–481
Preuss JMH, Rigby PJ, Goldie RG (1999) The influence of animal age and β-adrenoceptor density and function in tracheal airway smooth muscle. Naunyn-Schmiedeberg's Arch Pharmacol 360:171–178
Roffel AF, Elzinga CRS, van Amsterdam RGM, De Zeeuw RA, Zaagsma J (1988) Muscarinic M2 receptors in bovine tracheal smooth muscle: discrepancies between binding and function. Eur J Pharmacol 153:73–82
Roffel AF, Elzinga CRS, Zaagsma J (1990) Muscarinic M3 receptors mediate contraction of human central and peripheral airway smooth muscle. Pulm Pharmacol 3:47–51
Salpeter SR, Buckley NS, Ormiston TM, Salpeter EE (2006) Meta-analysis: effect of long-acting β-agonists on severe asthma exacerbations and asthma-related deaths. Ann Int Med 144:904–912
Sarria B, Naline E, Zhang Y, Cortijo J, Molimard M, Moreau J, Therond P, Advenier C, Morcillo EJ (2002) Muscarinic M2 receptors in acetylcholine-isoproterenol functional antagonism in human isolated bronchus. Am J Physiol 283:L1125–L1132
Scherer D, Kiesecker C, Kulzer M, Günth M, Scholz EP, Kathöfer S, Thomas D, Maurer M, Kreuzer J, Bauer A, Katus HA, Karle CA, Zitron E (2007) Activation of inwardly rectifying Kir2.x potassium channels by β3-adrenoceptors is mediated via different signaling pathways with a predominant role of PKC for Kir2.1 and of PKA for Kir2.2. Naunyn-Schmiedeberg's Arch Pharmacol 375:311–322
Schneider T, Fetscher C, Krege S, Michel MC (2004a) Signal transduction underlying carbachol-induced contraction of human urinary bladder. J Pharmacol Exp Ther 309:1148–1153
Schneider T, Hein P, Michel MC (2004b) Signal transduction underlying carbachol-induced contraction of rat urinary bladder. I. Phospholipases and Ca2 sources. J Pharmacol Exp Ther 308:47–53
Sney J, Tsaneva-Atanasova K, Reznikov V, Bai Y, Sanderson MJ, Yule DI (2003) A method for determining the dependence of calcium oscillations on inositol trisphosphates oscillations. Proc Natl Acad Sci USA 103:1675–1680
Somogyi GT, Tanowitz M, Zernova G, De Groat WC (1996) M1 muscarinic receptor-induced facilitation of ACh and noradrenaline release in the rat bladder is mediated by protein kinase C. J Physiol (London) 496:245–254
Stengel PW, Gomeza J, Wess J, Cohen ML (2000) M2 and M4 receptor knockout mice: muscarinic receptor function in cardiac and smooth muscle in vitro. J Pharmacol Exp Ther 292:877–885
Stengel PW, Yamada M, Wess J, Cohen ML (2002) M3-receptor knockout mice: muscarinic receptor function in atria, stomach fundus, urinary bladder, and trachea. Am J Physiol Regul Integr Comp Physiol 282:R1443–R1449
Struckmann N, Schwering S, Wiegand S, Gschnell A, Yamada M, Kummer W, Wess J, Haberberger RV (2003) Role of muscarinic receptor subtypes in the constriction of peripheral airways: studies on receptor-deficient mice. Mol Pharmacol 64:1444–1451
Szalai C, Ungvari I, Pelyhe L, Tölgyesi G, Falus A (2008) Asthma from a pharmacogenomic point of view. Br J Pharmacol 153:1602–1614
Tanaka Y, Yamashita Y, Michikawa H, Horinouchi T, Koike K (2007) Pharmacological characterization of the β-adrenoceptor that mediates the relaxant response to noradrenaline in guinea-pig tracheal smooth muscle. Naunyn-Schmiedeberg's Arch Pharmacol 375:51–64
Thakkinstian A, McEvoy M, Minelli C, Gibson P, Hancox B, Duffy D, Thompson J, Hall I, Kaufman J, Leung T, Helms PJ, Hakonarson H, Halpi E, Navon R, Attia J (2005) Systematic review and meta-analysis of the association between β2-adrenoceptor polymorphisms and asthma: a HuGE review. Am J Epidemiol 162:201–211
Tran JA, Matsui M, Ehlert FJ (2006) Differential coupling of muscarinic M1, M2, and M3 receptors to phosphoinositide hydrolysis in urinary bladder and longitudinal muscle of the ileum of the mouse. J Pharmacol Exp Ther 318:649–656
Tran TM, Friedman J, Baameur F, Knoll BJ, Moore RH, Clark RB (2007) Characterization of β2-adrenergic receptor dephosphorylation: comparison with the rate of resensitization. Mol Pharmacol 71:47–60
Trendelenburg A-U, Gomeza J, Klebroff W, Zhou H, Wess J (2003) Heterogeneity of presynaptic muscarinic receptors mediating inhibition of sympathetic transmitter release: a study with M2- and M4-receptor-deficient mice. Br J Pharmacol 138:469–480
Uchida H, Shishido K, Nomiya M, Yamaguchi O (2005) Involvement of cyclic AMP-dependent and -independent mechanisms in the relaxation of rat detrusor muscle via β-adrenoceptors. Eur J Pharmacol 518:195–202
Vrydag W, Michel MC (2007) Tools to study β3-adrenoceptors. Naunyn-Schmiedeberg's Arch Pharmacol 374:385–398
Vrydag W, Michel MC (2008) Agonist-induced desensitization of rat bladder relaxation by β-adrenergic agonists. FASEB J 22:916.5
Wegener JW, Schulla V, Lee T-S, Koller A, Feil S, Feil R, Kleppisch T, Klugbauer N, Moosmang S, Welling A, Hofmann F (2004) An essential role of CaV1.2 L-type calcium channel for urinary bladder function. FASEB J 18:1159–1161
Wessler IK, Kirkpatrick CJ (2001) The non-neuronal cholinergic system: an emerging drug target in the airways. Pulm Pharmacol Ther 14:423–434
Wuest M, Weiss A, Waelbrock M, Braeter M, Kelly L-U, Hakenberg OW, Ravens U (2006) Propiverine and metabolites: differences in binding to muscarinic receptors and in functional models of detrusor contraction. Naunyn-Schmiedeberg's Arch Pharmacol 374:87–97
Wuest M, Hiller N, Braeter M, Hakenberg OW, Wirth MP, Ravens U (2007) Contribution of Ca2 influx to carbachol-induced detrusor contraction is different in human urinary bladder compared to pig and mouse. Eur J Pharmacol 565:180–189
Zarghooni S, Wunsch J, Bodenbenner M, Brüggmann D, Grando SA, Schwantes U, Wess J, Kummer W, Lips KS (2007) Expression of muscarinic and nicotinic acetylcholine receptors in the mouse urothelium. Life Sci 80:2308–2313
Acknowledgement
Work in the authors’ laboratory on bladder function has been funded in part by the Deutsche Forschungsgemeinschaft, Astellas, Boehringer Ingelheim, Pfizer, and Theravance.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors wish to dedicate this manuscript to Prof. Hans Zaagsma on the occasion of his retirement.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Michel, M.C., Parra, S. Similarities and differences in the autonomic control of airway and urinary bladder smooth muscle. Naunyn-Schmied Arch Pharmacol 378, 217–224 (2008). https://doi.org/10.1007/s00210-008-0316-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-008-0316-5