Abstract
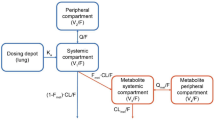
The precise assessment of the dose–response to bronchodilators in the treatment of chronic obstructive pulmonary disease is hindered by the low signal to noise ratio of the typical clinical endpoint FEV1. Kinetic-pharmacodynamic (K-PD) models which use time course of response over a range of doses are in principle suited for the assessment of the dose response relationship of pulmonary administered drugs. A K-PD model was successfully developed using the longitudinal FEV1 data collected in the clinical study for a novel bronchodilator X. A superposition of two cosine functions was selected to describe the circadian variability in FEV1 at baseline. The onset (ka) and offset (kde) of drug action were described with first-order rate constants of 0.214/h and 0.141/h, respectively. Drug potency, EKD50, was estimated as 6.56 μg/h, and the maximum response, Emax as 0.631 L. Between-subject variability for kde, EKD50 and Emax were 65, 84.7 or 34.4% (expressed as coefficient variation). The model-based simulation predicted that for the same total daily dose of once-daily and twice-daily regimens, the trough FEV1 response to a twice-daily regimen was higher, and the maximum FEV1 response to once-daily regimen was higher, while the predicted average FEV1 response was about the same.







Similar content being viewed by others
References
Chen X, Mallikaarjun S (2005) Modeling of circadian effect on lung function in patients with chronic obstructive pulmonary disease. PAGE
American Thoracic Society. Standardization of spirometry, 1994 update (1995). Am J Respir Crit Care Med 152:1107–1136
Gabrielsson J, Jusko W, Alari L (2000) Modeling of dose-response-time data: four examples of estimating the turnover parameters and generating kinetic functions from the response profiles. Biopharm Drug Dispos 21:41–52
Jacqmin P, Snoeck E, van Schaick EA, Gieschke R, Pillai P, Steimer JL, Girard P (2006) Modeling response time profiles in the absence of drug concentrations; definition and performance evaluation of the K-PD model. J Pharmacokinet Pharmacodyn 34:57–85
Pillai G, Gieschke R, Goggin T, Jacqmin P, Schimmer RC, Steimer JL (2004) A semimechanistic and mechanistic population PK–PD model for biomarker response to ibandronate, a new bisphosphonate for the treatment of osteoporosis. Br J Clin Pharmacol 58:618–631
Barnes PJ (1993) Muscarinic receptor subtypes in airways. Life Sci 52:521–528
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee (2001) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 163:1256–1276
Sheiner LB, Beal SL (1992) NONMEM user guide. University of California, San Francisco
Lindbom L, Pihlgren P, Jonsson EN (2005) PsN-Toolkit—a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 79:241–257
Holford N (2005) The visual predictive check—superiority to standard diagnostic (Rorschach) plots. PAGE
Karlsson MO, Sheiner LB (1993) The importance of modeling interoccasion variability in population pharmacokinetic analyses. J Pharmacokinet Pharmacodyn 21:735–750
Karlsson MO, Sheiner LB (1994) Estimating bioavailability when clearance varies with time. Clin Pharmacol Ther 55:623–637
Lalonde R, Ouellet D, Kimanani EK, Potvin D, Vaughan LM, Hill RM (1999) Comparison of different methods to evaluate population dose–response and relative potency: importance of interoccasion variability. J Pharmacokinet Pharmacodyn 27:67–83
Matthews I, Kirkpatrick C, Holford N (2004) Quantitative justification for target concentration intervention–parameter variability and predictive performance using population pharmacokinetic models for aminoglycosides. Br J Clin Pharmacol 58:8–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, K., Looby, M., Pillai, G. et al. Population pharmacodynamic model of the longitudinal FEV1 response to an inhaled long-acting anti-muscarinic in COPD patients. J Pharmacokinet Pharmacodyn 38, 105–119 (2011). https://doi.org/10.1007/s10928-010-9180-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-010-9180-2