Abstract
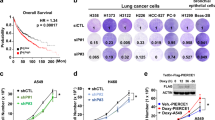
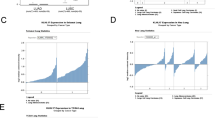
KRAS mutations are one of the most common driver mutations in non-small-cell lung cancer (NSCLC) and finding druggable target molecules to inhibit oncogenic KRAS signaling is a significant challenge in NSCLC therapy. We recently identified epiregulin (EREG) as one of several putative transcriptional targets of oncogenic KRAS signaling in both KRAS-mutant NSCLC cells and immortalized bronchial epithelial cells expressing ectopic mutant KRAS. In the current study, we found that EREG is overexpressed in NSCLCs harboring KRAS, BRAF or EGFR mutations compared with NSCLCs with wild-type KRAS/BRAF/EGFR. Small interfering RNAs (siRNAs) targeting mutant KRAS, but not an siRNA targeting wild-type KRAS, significantly reduced EREG expression in KRAS-mutant and EREG-overexpressing NSCLC cell lines. In these cell lines, EREG expression was downregulated by MEK and ERK inhibitors. Importantly, EREG expression significantly correlated with KRAS expression or KRAS copy number in KRAS-mutant NSCLC cell lines. Further expression analysis using 89 NSCLC specimens showed that EREG was predominantly expressed in NSCLCs with pleural involvement, lymphatic permeation or vascular invasion and in KRAS-mutant adenocarcinomas. In addition, multivariate analysis revealed that EREG expression is an independent prognostic marker and EREG overexpression in combination with KRAS mutations was associated with an unfavorable prognosis for lung adenocarcinoma patients. In KRAS-mutant and EREG overexpressing NSCLC cells, siRNA-mediated EREG silencing inhibited anchorage-dependent and -independent growth and induced apoptosis. Our findings suggest that oncogenic KRAS-induced EREG overexpression contributes to an aggressive phenotype and could be a promising therapeutic target in oncogenic KRAS-driven NSCLC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D . Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
Larsen JE, Minna JD . Molecular biology of lung cancer: clinical implications. Clin Chest Med 2011; 32: 703–740.
Devesa SS, Bray F, Vizcaino AP, Parkin DM . International lung cancer trends by histologic type: male:female differences diminishing and adenocarcinoma rates rising. Int J Cancer 2005; 117: 294–299.
Mascaux C, Iannino N, Martin B, Paesmans M, Berghmans T, Dusart M et al. The role of RAS oncogene in survival of patients with lung cancer: a systematic review of the literature with meta-analysis. Br J Cancer 2005; 92: 131–139.
Ding L, Getz G, Wheeler DA, Mardis ER, McLellan MD, Cibulskis K et al. Somatic mutations affect key pathways in lung adenocarcinoma. Nature 2008; 455: 1069–1075.
Suda K, Tomizawa K, Mitsudomi T . Biological and clinical significance of KRAS mutations in lung cancer: an oncogenic driver that contrasts with EGFR mutation. Cancer Metastasis Rev 2010; 29: 49–60.
Sunaga N, Shames DS, Girard L, Peyton M, Larsen JE, Imai H et al. Knockdown of oncogenic KRAS in non-small cell lung cancers suppresses tumor growth and sensitizes tumor cells to targeted therapy. Mol Cancer Ther 2011; 10: 336–346.
Toyoda H, Komurasaki T, Uchida D, Takayama Y, Isobe T, Okuyama T et al. Epiregulin. A novel epidermal growth factor with mitogenic activity for rat primary hepatocytes. J Biol Chem 1995; 270: 7495–7500.
Shelly M, Pinkas-Kramarski R, Guarino BC, Waterman H, Wang LM, Lyass L et al. Epiregulin is a potent pan-ErbB ligand that preferentially activates heterodimeric receptor complexes. J Biol Chem 1998; 273: 10496–10505.
Riese DJ, Komurasaki T, Plowman GD, Stern DF . Activation of ErbB4 by the bifunctional epidermal growth factor family hormone epiregulin is regulated by ErbB2. J Biol Chem 1998; 273: 11288–11294.
Toyoda H, Komurasaki T, Uchida D, Morimoto S . Distribution of mRNA for human epiregulin, a differentially expressed member of the epidermal growth factor family. Biochem J 1997; 326: 69–75.
Zhu Z, Kleeff J, Friess H, Wang L, Zimmermann A, Yarden Y et al. Epiregulin is up-regulated in pancreatic cancer and stimulates pancreatic cancer cell growth. Biochem Biophys Res Commun 2000; 273: 1019–1024.
Thogersen VB, Sorensen BS, Poulsen SS, Orntoft TF, Wolf H, Nexo E . A subclass of HER1 ligands are prognostic markers for survival in bladder cancer patients. Cancer Res 2001; 61: 6227–6233.
Nicholson BE, Frierson HF, Conaway MR, Seraj JM, Harding MA, Hampton GM et al. Profiling the evolution of human metastatic bladder cancer. Cancer Res 2004; 64: 7813–7821.
Fujimoto N, Wislez M, Zhang J, Iwanaga K, Dackor J, Hanna AE et al. High expression of ErbB family members and their ligands in lung adenocarcinomas that are sensitive to inhibition of epidermal growth factor receptor. Cancer Res 2005; 65: 11478–11485.
Revillion F, Lhotellier V, Hornez L, Bonneterre J, Peyrat JP . ErbB/HER ligands in human breast cancer, and relationships with their receptors, the bio-pathological features and prognosis. Ann Oncol 2008; 19: 73–80.
Zhang J, Iwanaga K, Choi KC, Wislez M, Raso MG, Wei W et al. Intratumoral epiregulin is a marker of advanced disease in non-small cell lung cancer patients and confers invasive properties on EGFR-mutant cells. Cancer Prev Res 2008; 1: 201–207.
Wang X, Colby JK, Rengel RC, Fischer SM, Clinton SK, Klein RD . Overexpression of cyclooxygenase-2 (COX-2) in the mouse urinary bladder induces the expression of immune- and cell proliferation-related genes. Mol Carcinog 2009; 48: 1–13.
Sun M, Behrens C, Feng L, Ozburn N, Tang X, Yin G et al. HER family receptor abnormalities in lung cancer brain metastases and corresponding primary tumors. Clin Cancer Res 2009; 15: 4829–4237.
Takahashi M, Hayashi K, Yoshida K, Ohkawa Y, Komurasaki T, Kitabatake A et al. Epiregulin as a major autocrine/paracrine factor released from ERK- and p38MAPK-activated vascular smooth muscle cells. Circulation 2003; 108: 2524–2529.
Cho MC, Choi HS, Lee S, Kim BY, Jung M, Park SN et al. Epiregulin expression by Ets-1 and ERK signaling pathway in Ki-ras-transformed cells. Biochem Biophys Res Commun 2008; 377: 832–837.
Soh J, Okumura N, Lockwood WW, Yamamoto H, Shigematsu H, Zhang W et al. Oncogene mutations, copy number gains and mutant allele specific imbalance (MASI) frequently occur together in tumor cells. PLoS One 2009; 4: e7464.
Pratilas CA, Hanrahan AJ, Halilovic E, Persaud Y, Soh J, Chitale D et al. Genetic predictors of MEK dependence in non-small cell lung cancer. Cancer Res 2008; 68: 9375–9383.
Marchetti A, Felicioni L, Malatesta S, Grazia Sciarrotta M, Guetti L, Chella A et al. Clinical features and outcome of patients with non-small-cell lung cancer harboring BRAF mutations. J Clin Oncol 2011; 29: 3574–3579.
Baba I, Shirasawa S, Iwamoto R, Okumura K, Tsunoda T, Nishioka M et al. Involvement of deregulated epiregulin expression in tumorigenesis in vivo through activated Ki-Ras signaling pathway in human colon cancer cells. Cancer Res 2000; 60: 6886–6889.
Lee S, Kang J, Cho M, Seo E, Choi H, Kim E et al. Profiling of transcripts and proteins modulated by K-ras oncogene in the lung tissues of K-ras transgenic mice by omics approaches. Int J Oncol 2009; 34: 161–172.
Chu EK, Foley JS, Cheng J, Patel AS, Drazen JM, Tschumperlin DJ . Bronchial epithelial compression regulates epidermal growth factor receptor family ligand expression in an autocrine manner. Am J Respir Cell Mol Biol 2005; 32: 373–380.
Regales L, Gong Y, Shen R, de Stanchina E, Vivanco I, Goel A et al. Dual targeting of EGFR can overcome a major drug resistance mutation in mouse models of EGFR mutant lung cancer. J Clin Invest 2009; 119: 3000–3010.
Phelps RM, Johnson BE, Ihde DC, Gazdar AF, Carbone DP, McClintock PR et al. NCI-Navy Medical Oncology Branch cell line data base. J Cell Biochem Suppl 1996; 24: 32–91.
Yamamoto H, Shigematsu H, Nomura M, Lockwood WW, Sato M, Okumura N et al. PIK3CA mutations and copy number gains in human lung cancers. Cancer Res 2008; 68: 6913–6921.
Draper BK, Komurasaki T, Davidson MK, Nanney LB . Epiregulin is more potent than EGF or TGFalpha in promoting in vitro wound closure due to enhanced ERK/MAPK activation. J Cell Biochem 2003; 89: 1126–1137.
Lindvall C, Hou M, Komurasaki T, Zheng C, Henriksson M, Sedivy JM et al. Molecular characterization of human telomerase reverse transcriptase-immortalized human fibroblasts by gene expression profiling: activation of the epiregulin gene. Cancer Res 2003; 63: 1743–1747.
Zhao M, He HW, Sun HX, Ren KH, Shao RG . Dual knockdown of N-ras and epiregulin synergistically suppressed the growth of human hepatoma cells. Biochem Biophys Res Commun 2009; 387: 239–244.
Gupta GP, Nguyen DX, Chiang AC, Bos PD, Kim JY, Nadal C et al. Mediators of vascular remodelling co-opted for sequential steps in lung metastasis. Nature 2007; 446: 765–770.
Hu K, Li SL, Gan YH, Wang CY, Yu GY . Epiregulin promotes migration and invasion of salivary adenoid cystic carcinoma cell line SACC-83 through activation of ERK and Akt. Oral Oncol 2009; 45: 156–163.
Gazdar AF, Minna JD . Deregulated EGFR signaling during lung cancer progression: mutations, amplicons, and autocrine loops. Cancer Prev Res 2008; 1: 156–160.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009; 361: 947–957.
Morita S, Okamoto I, Kobayashi K, Yamazaki K, Asahina H, Inoue A et al. Combined survival analysis of prospective clinical trials of gefitinib for non-small cell lung cancer with EGFR mutations. Clin Cancer Res 2009; 15: 4493–4498.
Pao W, Wang TY, Riely GJ, Miller VA, Pan Q, Ladanyi M et al. KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med 2005; 2: e17.
Massarelli E, Varella-Garcia M, Tang X, Xavier AC, Ozburn NC, Liu DD et al. KRAS mutation is an important predictor of resistance to therapy with epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. Clin Cancer Res 2007; 13: 2890–2896.
Gandhi J, Zhang J, Xie Y, Soh J, Shigematsu H, Zhang W et al. Alterations in genes of the EGFR signaling pathway and their relationship to EGFR tyrosine kinase inhibitor sensitivity in lung cancer cell lines. PLoS One 2009; 4: e4576.
Kris M, Johnson BE, Kwiatkowski DJ, Iafrate AJ, Wistuba II, Aronson SL et al. Identification of driver mutations in tumor specimens from 1000 patients with lung adenocarcinoma: the NCI’s lung cancer mutation consortium (LCMC). J Clin Oncol 2011; 29: (Suppl; abstract CRA7506).
Gazdar AF . Activating and resistance mutations of EGFR in non-small-cell lung cancer: role in clinical response to EGFR tyrosine kinase inhibitors. Oncogene 2009; 28: S24–S31.
Imai H, Sunaga N, Shimizu Y, Kakegawa S, Shimizu K, Sano T et al. Clinicopathological and therapeutic significance of CXCL12 expression in lung cancer. Int J Immunopathol Pharmacol 2010; 23: 153–164.
Sunaga N, Imai H, Shimizu K, Shames DS, Kakegawa S, Girard L et al. Oncogenic KRAS-induced interleukin-8 overexpression promotes cell growth and migration and contributes to aggressive phenotypes of non-small cell lung cancer. Int J Cancer 2012; 130: 1733–1744.
Sunaga N, Miyajima K, Suzuki M, Sato M, White MA, Ramirez RD et al. Different roles for caveolin-1 in the development of non-small cell lung cancer versus small cell lung cancer. Cancer Res 2004; 64: 4277–4285.
Kaira K, Endo M, Abe M, Nakagawa K, Ohde Y, Okumura T et al. Biologic correlation of 2-[18F]-fluoro-2-deoxy-D-glucose uptake on positron emission tomography in thymic epithelial tumors. J Clin Oncol 2010; 28: 3746–3753.
Acknowledgements
This work was supported by Grants-in-Aid for Scientific Research (C) (grant #23591134) from the Japan Society for the Promotion of Science. Funding for this work also came from SPORE (P50CA70907); DOD PROSPECT, Texas Higher Education Coordinating Board Advanced Technology Program (grant #01001901392003); Gillson Longenbaugh Foundation; NASA Specialized Center of Research (grant #NNJ05HD36G). We thank Drs Yoshio Tomizawa, Noriko Yanagitani, Hironobu Iijima, Takeshi Hisada, Mitsuyoshi Utsugi of the Department of Medicine and Molecular Science, Gunma University Graduate School of Medicine, Gunma, Japan for technical support and critical advices. We also thank Drs Kenneth Huffman and Victor Stastny of the Hamon Center for Therapeutic Oncology Research, University of Texas Southwestern Medical Center at Dallas for kind assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Oncogene website
Supplementary information
Rights and permissions
About this article
Cite this article
Sunaga, N., Kaira, K., Imai, H. et al. Oncogenic KRAS-induced epiregulin overexpression contributes to aggressive phenotype and is a promising therapeutic target in non-small-cell lung cancer. Oncogene 32, 4034–4042 (2013). https://doi.org/10.1038/onc.2012.402
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2012.402
Keywords
This article is cited by
-
A novel selective ERK1/2 inhibitor, Laxiflorin B, targets EGFR mutation subtypes in non-small-cell lung cancer
Acta Pharmacologica Sinica (2024)
-
Low Dose of Green Synthesized Silver Nanoparticles is Sufficient to Cause Strong Cytotoxicity via its Cytotoxic Efficiency and Modulatory Effects on the Expression of PIK3CA and KRAS Oncogenes, in Lung and Cervical Cancer Cells
Journal of Cluster Science (2023)
-
3-Nitrobenzanthrone promotes malignant transformation in human lung epithelial cells through the epiregulin-signaling pathway
Cell Biology and Toxicology (2022)
-
Depletion of EREG enhances the osteo/dentinogenic differentiation ability of dental pulp stem cells via the p38 MAPK and Erk pathways in an inflammatory microenvironment
BMC Oral Health (2021)
-
The miR-186-3p/EREG axis orchestrates tamoxifen resistance and aerobic glycolysis in breast cancer cells
Oncogene (2019)