Abstract
Objective
To evaluate whether a β2-adrenergic agonist may reduce acute alveolo-capillary barrier alterations during high-volume ventilation.
Design
Experimental study.
Setting
Animal research laboratory.
Subjects
A total of 48 male Wistar rats.
Interventions
A zone of alveolar flooding was produced by liquid instillation in a distal airway. Proteins in the instilled solution were traced with 99mTc-albumin. 111In, which binds to transferrin, was injected into the systemic circulation. Terbutaline was administered in the instilled solution or intra-peritoneally. Conventional ventilation was applied for 30 min followed by different ventilation strategies for 90 min: conventional ventilation, high-volume ventilation with or without 6 cmH2O PEEP.
Measurements and main results
Protein fluxes across the alveolar and microvascular barriers were evaluated by scintigraphy. High-volume ventilation resulted in immediate leakage of 99mTc-albumin from alveolar spaces and increased pulmonary uptake of systemic 111In-transferrin. Terbutaline in the instilled solution and PEEP lessened alveolar 99mTc-albumin leakage and pulmonary 111In-transferrin uptake due to high-volume ventilation, whereas terbutaline given intra-peritoneally only lessened 111In-transferrin uptake. Terbutaline in the instilled solution also lessened the increase in lung wet-to-dry weight ratio due to high-volume ventilation.
Conclusions
Terbutaline reduces protein fluxes across the alveolar epithelial and pulmonary microvascular barriers during high-volume ventilation in vivo. The route of administration may be important.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS), the most severe form of acute lung injury, is characterized by a permeability-type pulmonary edema resulting in severe life-threatening hypoxemia [1]. Experimental studies suggested that unnecessary lung tissue stress could have played a role in the poor prognosis of this diseased state [2]. As a matter of fact, reducing the mechanical stress applied to the lungs by lowering tidal volume from 12 to 6 ml/kg improved the survival of ARDS patients by 22% [3]. However, the overall prognosis of acute lung injury remains poor, with mortality rates ranging from 15% to 60% depending on patient age [4].
Pharmacological therapies have been tested for many years in ARDS patients, but none of them have improved survival [5]. A randomized placebo-controlled trial showed that prophylactic inhalation of salmeterol, a long-acting β2-agonist, decreased by 50% the incidence of high-altitude pulmonary edema in volunteers known to be at risk [6]. A randomized trial recently suggested that salbutamol infusion might lessen plateau airway pressure and decrease extravascular lung water in ARDS patients [7]. The protective effect of β2-adrenergic agonists may be related in part to increased alveolar liquid clearance [8], but perhaps also to the lessening of microvascular and/or alveolar permeability alterations that accompany permeability-type pulmonary edema [9]. Beta-adrenergic agonist infusion reduced endothelial permeability in a model of acid-induced lung injury [10] and pulmonary edema in an ovine model of burn and smoke inhalation [11], indicating that it decreased transvascular fluid flux. Basran et al. [12] found that terbutaline infusion reduced accumulation of plasma protein in the lungs of ARDS patients, which suggested that it might have lessened microvascular permeability alterations.
Whether β2-adrenergic agonists may similarly lessen the increase in alveolar permeability produced by mechanical stress is unknown. Parker et al. [13] showed that isoproterenol attenuated microvascular permeability increase due to high transmural microvascular pressures in isolated rat lungs. However, improving permeability on one side of the barrier may be offset by an absence of improvement on the other side, because the responses of the epithelial and endothelial layers sometimes differ [14]. Therefore, we used a previously validated model based on scintigraphic imaging [15] to non-invasively study the effect of a β2-adrenergic agonist on protein fluxes across the alveolo-capillary barrier during high-volume ventilation.
Material and methods
Animals
All experiments were conducted in compliance with the recommendations for laboratory animal research of the European Union and the French Ministry of Agriculture. Male Wistar rats (n = 48, weighing 295–345 g, Elevage Janvier, Le Genest Saint Isle, France) were anesthetized by intra-peritoneal injection of 50 mg/kg pentobarbital (Sigma, St Quentin Fallavier, France). They were tracheotomized and a cannula (Braun, Melsungen, Germany) was tightly secured to the trachea to avoid gas leaks.
Ventilation modalities
Rats were paralyzed by injection of 15 mg/kg succinyl-choline (Sigma) and ventilated using a Harvard rodent volume ventilator (Ealing, Courtaboeuf, France). Additional 10 mg/kg pentobarbital injections were performed every 30 min. Rats not injected with succinyl-choline had no nociceptive reaction with this protocol. Conventional ventilation (CV; 8 ml/kg VT, PEEP 2 cmH2O, respiratory rate 70/min) was applied for 30 min, followed by different ventilation modalities for 90 min. Several ventilation modalities were tested: CV, high-volume ventilation (HV) at 30 cmH2O end-inspiratory pressure (Pei) and no PEEP (HV1) and HV with PEEP set at 6 cmH2O (HV1P) and VT adjusted to be about the same (25 ml/kg) as during HV1. This latter ventilation modality resulted in a slightly higher Pei (Table 1). Pei during HV was very close to plateau pressure considering the low respiratory rate and the shape of the ventilator waveform, which was nearly sinusoidal [16]. A less injurious strategy was used when terbutaline was given intra-peritoneally (IP; see below), in order to increase sensitivity. Pei was set at 25 cmH2O (HV2), which was shown to increase permeability [15], respiratory rate being set the same as during 30 cmH2O Pei ventilation. During these experiments a catheter was placed in a carotid artery and arterial pressure was measured using a Statham pressure transducer and registered at 15-min intervals.
Scintigraphic imaging
Scintigraphic imaging was performed as previously described [15]. Briefly, continuous planar thoracic acquisitions were performed (γ Imager, Biospace, Paris, France) that lasted 120 min without interruption. Dynamic series of images of 150 s each were computed from the registered scintigraphy data.
Measurement of microvascular and epithelial permeability
Pulmonary microvascular permeability was estimated by the rate of 111In-transferrin accumulation in lungs relative to heart. About 400 μCi of 111In chloride (indium strongly binds to transferrin in vivo) were injected in the dorsal penile vein. Regions of interest (ROI) were delineated on the cardiac cavities using the early images and on the zones corresponding to the instilled and contralateral lung (ROIE and ROICL). 111In-transferrin accumulation rate was deduced from the normalized lung to heart activity ratio [17]. 111In-transferrin accumulation slope was calculated by linear regression.
Alveolar epithelial permeability to albumin was obtained from the rate at which 99mTc-labeled albumin leaked from the lungs. 99mTc-labeled albumin was prepared using a commercial kit (Vasculocis; Cis Bio International, Gif sur Yvette, France). Two hundred and fifty microliters of an × 2 hypertonic mannitol solution (120 mg/ml), supplemented with bovine serum albumin (80 mg/ml), sodium transport inhibitors and 600 μCi 99mTc-albumin [15], were instilled in one lung so that pulmonary microvascular permeability could be compared between the instilled and the uninstilled lung. The solution was slowly instilled in a distal airway after a short period of ventilation with FiO2 = 1. β2-Aadrenergic stimulation was done adding 10−4M (approximately 0.02 mg/kg body weight) terbutaline to the instillate (intra-tracheally, IT), or injecting 0.5 mg/kg IP, immediately before the initial CV period. 99mTc activity in a ROI drawn over the thorax (ROIT) was integrated over 150-s steps and divided by initial activity. We have shown [15] that the initial decay slope, measured during the first 6 min of change in lung 99mTc-albumin content, was proportional to alveolar albumin permeability–surface area product (PSA).
Wet-to-dry lung ratios
After the rats were killed with an overdose of pentobarbital, the trachea was clamped. The thorax was opened and the main bronchi tied. The lungs were weighed and placed at −20 °C for 30 days to allow radioactivity to decay. They were then again weighed to verify the absence of significant weight loss and weighed dry after being left at 80 °C for 7 days.
Statistical analysis
Results are expressed as mean ± SEM. Comparisons between groups were made by one or two-way ANOVA and the Bonferroni post-hoc test, or by the Kruskal–Wallis test and the Dunn post-hoc test. A probability value of p < 0.05 or less was considered significant (Prism; GraphPad, San Diego, USA).
Results
End-inspiratory pressure during ventilation
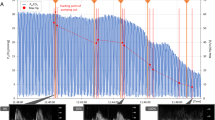
The Pei values at t30 (end of the baseline CV period) and later are shown in Fig. 1. Pei remained steady in the CV groups. It increased when 30 cmH2O Pei ventilation was initiated, but significantly less in the presence of terbutaline (p < 0.001 at 90 and 120 min). Pei remained steady in the presence of PEEP, and even decreased to be significantly lower at 120 min (p < 0.001) when terbutaline was given IT. After an initial increase, Pei remained steady during HV at 25 cmH2O Pei whether terbutaline was given IP or not.
Changes in end-inspiratory pressure (Pei) during ventilation with terbutaline (T) given in the instillate (intra-tracheally, IT) or intra-peritoneally (IP) or without terbutaline. Pei was similar in all groups during the 30-min conventional ventilation (CV) period and stayed low in animals ventilated with this modality. Pei increased sharply in rats ventilated with a high volume at 30 cmH2O Pei (HV1), either in the absence or the presence of PEEP (HV2P), but not at 25 cmH2O Pei and no PEEP (HV2). Intra-tracheal terbutaline significantly decreased Pei in animals ventilated at 30 cmH2O Pei (p < 0.001 at 90 and 120 min)
Mean arterial pressure and heart rate
Mean arterial pressure (MAP) decreased and heart rate (HR) increased almost immediately after terbutaline was given IP. MAP was lower in rats given terbutaline IP at the beginning of the HV period (Table 1) and remained lower than in similarly ventilated controls during all this period (p < 0.001 by two-way ANOVA), although it had a slight tendency to increase with time. HR was significantly higher at the beginning of the CV period in rats given terbutaline IP (401 ± 19.7 vs 311 ± 22.0 bpm, p < 0.01). HR decreased after commencement of HV in both groups (Table 1), then remained steady and higher in rats given terbutaline IP than in controls during the whole HV period (p < 0.001 by two-way ANOVA).
Lung 111In-transferrin accumulation
Figure 2 shows that 111In-transferrin accumulated slowly in the lungs of rats ventilated with CV. The increase in 111In-transferrin accumulation rate was almost immediate when HV was applied. Terbutaline IT significantly lessened 111In-transferrin accumulation rate in the instilled and the contralateral lung. The decrease observed with terbutaline IP reached significance in the instilled lung only (Fig. 3). PEEP decreased lung 111In-transferrin accumulation (p < 0.01) to a value that was not significantly different from CV controls in uninstilled lungs (Fig. 3). The effect of terbutaline IT in the instilled lung did not reach significance.
Changes in 111In-transferrin lung/heart ratio in the region of interest drawn around the non-instilled lung during conventional ventilation (open circles), high-volume ventilation at 30 cmH2O end-inspiratory pressure without PEEP (open squares) applied at t = 30 min and the same ventilation modality in animals given terbutaline in the instillate (filled squares). Terbutaline significantly lessened the slope of lung/heart ratio increase (p < 0.001). The same observation was made for the flooded lung, or in both lungs in the presence of PEEP
Slopes of lung/heart ratio changes with and without terbutaline according to the ventilation modality – conventional ventilation (CV) or high-volume ventilation at 30 cmH2O end-inspiratory pressure without (HV1) or with PEEP (HV1P) – in the regions of interest drawn around the instilled (E, edema) and contralateral (CL) lung (pooled values). Terbutaline given in the instillate (intra-tracheally, IT) decreased lung/heart ratio slope in both lungs during HV1 (*** p < 0.001 compared with the same ventilation modality in the absence of terbutaline). Terbutaline given intra-peritoneally (IP) significantly decreased lung/heart ratio slope in the flooded lung during ventilation at 25 cmH2O end-inspiratory pressure (HV2; * p < 0.05 compared with the same ventilation modality in the absence of terbutaline)
Alveolar 99mTc-albumin permeability
CV was not accompanied by significant 99mTc-albumin leakage from airspaces. Terbutaline IT had no effect on albumin permeability during CV. HV produced an immediate decrease in lung 99mTc-albumin content, as previously reported [15], which was lessened by PEEP (Fig. 4, p < 0.01). Terbutaline IT significantly reduced the increase in albumin permeability due to HV ventilation, regardless of the presence of PEEP, as shown in Fig. 5. Albumin permeability in the presence of PEEP + terbutaline IT was higher, but not significantly so, than that in CV controls. Terbutaline IP did not affect the increase in alveolar albumin permeability due to 25 cmH2O Pei ventilation.
Changes in lung 99mTc-albumin content (pooled values) during conventional ventilation (open circles), high-volume ventilation at 30 cmH2O without PEEP (open squares) and the same ventilation modality in animals given terbutaline in the instillate (filled squares). Terbutaline lessened the leakage of albumin from alveolar spaces produced by high-volume ventilation. The same observation was made during high-volume ventilation with PEEP. Terbutaline given intra-peritoneally did not change alveolar albumin leakage
Alveolar 99mTc-albumin permeability surface area product (PSA, log scale) calculated from the initial slopes of the curves shown in Fig. 4. PSA was nearly 1,000 times higher (p < 0.001) during high-volume ventilation at 30 (HV1) or 25 cmH2O (HV2) end-inspiratory pressure than during conventional (CV) ventilation, irrespective of the presence of PEEP (HV1P). Terbutaline given in the instillate (intra-tracheally, IT), but not intra-peritoneally (IP), reduced PSA when increased by high-volume ventilation (*p < 0.05 compared with the same ventilation modality)
Wet-to-dry lung weight ratio
Wet-to-dry lung weight ratios are shown in Fig. 6. Terbutaline IT did not affect wet-to-dry ratio in the CV group. High-volume ventilation at 30 cmH2O (HV1) or 25 cmH2O (HV2) end-inspiratory pressure (Pei) significantly increased wet-to-dry ratio (p < 0.001). This increase was lessened by PEEP (HV1P, p < 0.05). Terbutaline IT significantly lessened wet-to-dry ratio in rats ventilated with 30 cmH2O Pei and ZEEP (HV1). Terbutaline IP did not affect this ratio during 25 cmH2O Pei ventilation and ZEEP.
Lung wet-to-dry ratios after conventional ventilation (CV), and high-volume ventilation at 30 cmH2O end-inspiratory pressure without (HV1) and with (HV1P) PEEP and high-volume ventilation at 25 cmH2O end-inspiratory pressure without PEEP (HV2). Wet-to-dry ratios were significantly lower when terbutaline was given in the instillate (intra-tracheally, IT), but not when it was given intra-peritoneally (IP). PEEP significantly lessened wet-to-dry ratios, independently of the presence of terbutaline IT. * p < 0.05
Discussion
This study shows that terbutaline, given either IT or IP, reduces protein fluxes across the capillary barrier during HV in vivo. Terbutaline IT, but not terbutaline IP, lessened the increase in alveolar permeability due to HV. This lessening was additive to that produced by PEEP. This is the first description, to our knowledge, of an effect of a β2-adrenergic agonist on alveolar epithelial permeability alterations due to high lung stretch.
Terbutaline and microvascular permeability alterations
Rats ventilated with CV slowly accumulated 111In-transferrin in their lungs, whether or not terbutaline was administered IT. HV at 25 or 30 cmH2O Pei produced a considerable increase in 111In-transferrin lung accumulation. We have shown that lung 111In-transferrin uptake increased when end-inspiratory pressure exceeded 20–25 cmH2O in rats [15, 18, 19]. This uptake was similar in aerated or flooded lungs because both experienced comparable distension at these airway pressures [15]. An increase in 111In-transferrin lung-to-heart ratio might also have been due to an increased lung blood volume. However, it is unlikely that HV would have produced a linear increase for at least 30 min, as shown in Fig. 2. Besides, microvascular permeability alterations during HV are well documented [2].
Ventilation with a high VT and no PEEP dispersed variable amounts of the instilled liquid, and thus terbutaline, in the uninstilled lung, which helps to explain why 111In-transferrin uptake was lessened in both lungs when terbutaline was given IT. PEEP application during HV reduced microvascular permeability, which even returned to control levels in the uninstilled lung [19]. This effect of PEEP provides a further explanation for the previous observations that PEEP lessened HV-induced pulmonary edema [20, 21] and lung albumin uptake [20].
The observation that terbutaline either given IT or IP reduces in vivo the HV-induced 111In-transferrin accumulation in the lungs agrees with previous observations made ex vivo showing that β-agonists lessen microvascular permeability alterations [13, 22]. Terbutaline may also have reduced filtration pressure, because of its relaxing effect on vasculature, which resulted in a significant MAP decrease when given IP. However, terbutaline is also inotropic; the increase in cardiac output usually seen with this agent in rats (see for example [23]) may have offset the consequences of this vasodilation on mean pulmonary capillary pressure. Although a decrease in mean capillary pressure cannot be excluded as an explanation for the decrease in pulmonary 111In-transferrin accumulation with terbutaline, it is likely that a lessening of permeability alterations also participated in this decrease. Indeed, the lessening of microvascular permeability by β-adrenergic agonists has been observed in various situations [10, 13, 24–26]. Interestingly, in the above-mentioned study by Basran et al. [12], five of the six patients in whom lung 113mIn-transferrin uptake was lower after terbutaline infusion survived, while the other four patients died.
Terbutaline and 99mTc-albumin alveolar permeability
Albumin clearance rate during CV was less than 2%/h, in keeping with previous estimates [15, 27]. This baseline clearance rate was unaffected by terbutaline. HV almost immediately increased PSA; PEEP application reduced this increase, as previously reported [19], despite slightly higher end-inspiratory (plateau) pressures, and thus comparable levels of overall lung distension. Terbutaline IT attenuated the increase in PSA whatever the level of PEEP. This effect was not limited to the early leakage of albumin from airspaces to the circulation (the data used to calculate PSA), but lasted at least 90 min, even in the absence of PEEP. It has been shown that PEEP application may help to prevent epithelial lesions during ventilation [20] perhaps by lessening abrasion due to liquid movement in airways [28–30], but these injuries occur later because relatively short periods of HV do not damage the lungs [31, 32]. Our observations suggests that β2-adrenergic agonists, when given IT, may combine with PEEP to prevent the HV-induced increase in alveolar/airway protein permeability. The route of terbutaline administration may, however, be important, at least in rats, because terbutaline given IP did not reduce the HV-induced increase in permeability. The administered dose was rather high, was proven effective in other models [33], and may even be harmful in rats [34]. Terbutaline IP produced significant systemic effects, a sustained decrease in MAP and increase in HR, and a reduction in pulmonary 111In-transferrin accumulation. It is thus possible that terbutaline did not reach alveolar cell β2-receptors at a sufficiently high concentration, as its effects were obvious when given IT. The issue of terbutaline dosage when administered in the systemic circulation deserves further studies.
Alveolar barrier permeability and lung water content
A recent randomized placebo-controlled trial showed that salbutamol infusion might decrease extravascular lung water in ALI or ARDS patients [7]. Because thermal dilution is a questionable method for measuring lung water in these patients [35], experimental studies are required to better evaluate whether β-adrenergic agonists really decrease lung water during permeability-type edema.
Our wet-to-dry ratio measurements suggest that β2-adrenergic agonist administration may slow pulmonary edema development during HV. Microvascular permeability alterations are the main determinant of pulmonary edema during ventilator-induced lung injury [2]. Microvascular protein reflection coefficient (and thus permeability) correlates with the rate of liquid extravasation at a given filtration pressure. It is therefore not surprising that the lessening of protein permeability alteration by β2-adrenergic treatment also affects wet-to-dry ratio.
It is possible that the protective effects of terbutaline observed in this study were due to hemodynamic changes. However, terbutaline is inotropic and increases cardiac output in the rat [23], so that it is difficult to infer from a decrease in MAP what occurred in the pulmonary microcirculation.
Another mechanism by which terbutaline might have decreased lung water content is stimulation of alveolar fluid clearance. Ware and Matthay have shown that alveolar liquid clearance is important for recovery in patients with ALI [8]. β-Adrenergic agonists have long been known to stimulate alveolar liquid clearance in the rat [36]. It is possible that the increase in permeability due to HV had facilitated leakage of transport inhibitors (which are small molecules) from the airspaces and increased sodium entry, and thus that alveolar liquid clearance was not completely inhibited when permeability was high. Few studies have considered the relationship between alveolar epithelium permeability and alveolar liquid clearance. Injuries that markedly increase alveolar permeability to proteins, such as severe Pseudomonas pneumonia, also decrease clearance [37]. However, it is likely that epithelial lesions are inhomogeneously distributed, so that alveolar clearance may be preserved in places. The observed decrease in wet-to-dry ratio observed with terbutaline IT may thus be related to the slowing of pulmonary edema development because of its protective effect on capillary barrier permeability and of liquid clearance stimulation. Terbutaline IP, which did not prevent alveolar permeability alterations, failed to lessen wet-to-dry ratio, which suggests that a preserved epithelium is essential to decrease the rate of edema formation. Whatever the mechanism, terbutaline IT offered a protection that was additive to that provided by PEEP.
In conclusion, this study shows that terbutaline IT reduces edema formation, possibly by lessening microvascular permeability alterations, during an injurious, high-volume, ventilation modality, and decreases the rate of edema formation in vivo. Terbutaline given IP seems less efficient than given IT in the rat. We were surprised to find no effect on alveolar permeability or lung water. We have no clear explanation for this observation. More work is needed to clarify the effect of terbutaline and of its route of administration on pulmonary transvascular protein fluxes in vivo during high lung stretch. However, beta-adrenergic agonists have been studied for several decades for their possible benefit during permeability type pulmonary edema/acute lung injury, but this issue has not so far received a definitive answer despite many studies [38]. Our study is the first to deal with the effect of a beta-adrenergic agonist on alveolar permeability changes, an effect that cannot be explained by hemodynamic alterations. The effects of terbutaline IT are additive to those of PEEP, suggesting that combination of both treatments may be beneficial to patients with acute lung injury and ARDS.
References
Ware LB, Matthay MA (2005) Clinical practice. Acute pulmonary edema. N Engl J Med 353:2788–2796
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med. 353:1685–1693
Cepkova M, Matthay MA (2006) Pharmacotherapy of acute lung injury and the acute respiratory distress syndrome. J Intensive Care Med 21:119–143
Sartori C, Allemann Y, Duplain H, Lepori M, Egli M, Lipp E, Hutter D, Turini P, Hugli O, Cook S, Nicod P, Scherrer U (2002) Salmeterol for the prevention of high-altitude pulmonary edema. N Engl J Med 346:1631–1636
Perkins GD, McAuley DF, Thickett DR, Gao F (2006) The beta-agonist lung injury trial (BALTI): a randomized placebo-controlled clinical trial. Am J Respir Crit Care Med 173:281–287
Ware LB, Matthay MA (2001) Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1376–1383
Montaner JS, Tsang J, Evans KG, Mullen JB, Burns AR, Walker DC, Wiggs B, Hogg JC (1986) Alveolar epithelial damage. A critical difference between high pressure and oleic acid-induced low pressure pulmonary edema. J Clin Invest 77:1786–1796
McAuley DF, Frank JA, Fang X, Matthay MA (2004) Clinically relevant concentrations of beta2-adrenergic agonists stimulate maximal cyclic adenosine monophosphate-dependent airspace fluid clearance and decrease pulmonary edema in experimental acid-induced lung injury. Crit Care Med 32:1470–1476
Palmieri TL, Enkhbaatar P, Bayliss R, Traber LD, Cox RA, Hawkins HK, Herndon DN, Greenhalgh DG, Traber DL (2006) Continuous nebulized albuterol attenuates acute lung injury in an ovine model of combined burn and smoke inhalation. Crit Care Med 34:1719–1724
Basran GS, Hardy JG, Woo SP, Ramasubramanian R, Byrne AJ (1986) Beta-2-adrenoceptor agonists as inhibitors of lung vascular permeability to radiolabelled transferrin in the adult respiratory distress syndrome in man. Eur J Nucl Med 12:381–384
Parker JC, Ivey CL (1997) Isoproterenol attenuates high vascular pressure-induced permeability increases in isolated rat lungs. J Appl Physiol 83:1962–1967
Frank JA, McAuley DF, Gutierrez JA, Daniel BM, Dobbs L, Matthay MA (2005) Differential effects of sustained inflation recruitment maneuvers on alveolar epithelial and lung endothelial injury. Crit Care Med 33:181–188
de Prost N, Dreyfuss D, Saumon G (2007) Evaluation of two-way protein fluxes across the alveolo-capillary membrane by scintigraphy in rats: effect of lung inflation. J Appl Physiol 102:794–802
Martin-Lefevre L, Ricard JD, Roupie E, Dreyfuss D, Saumon G (2001) Significance of the changes in the respiratory system pressure–volume curve during acute lung injury in rats. Am J Respir Crit Care Med 164:627–632
Roselli RJ, Riddle WR (1989) Analysis of noninvasive macromolecular transport measurements in the lung. J Appl Physiol 67:2343–2350
Bouvet F, Dreyfuss D, Lebtahi R, Martet G, Le Guludec D, Saumon G (2005) Noninvasive evaluation of acute capillary permeability changes during high-volume ventilation in rats with and without hypercapnic acidosis. Crit Care Med 33:155–160
de Prost N, Roux D, Dreyfuss D, Ricard JD, Le Guludec D, Saumon G (2007) Alveolar edema dispersion and alveolar protein permeability during high volume ventilation: effect of positive end-expiratory pressure. Intensive Care Med 33:711–717
Dreyfuss D, Basset G, Soler P, Saumon G (1985) Intermittent positive-pressure hyperventilation with high inflation pressures produces pulmonary microvascular injury in rats. Am Rev Respir Dis 132:880–884
Webb HH, Tierney DF (1974) Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 110:556–565
Parker JC (2000) Inhibitors of myosin light chain kinase and phosphodiesterase reduce ventilator-induced lung injury. J Appl Physiol 89:2241–2248
Poo JL, Braillon A, Hadengue A, Gaudin C, Lebrec D (1992) Hemodynamic effects of terbutaline, a beta 2-adrenoceptor agonist, in conscious rats with secondary biliary cirrhosis. Hepatology 15:459–463
Minnear FL, DeMichele MA, Leonhardt S, Andersen TT, Teitler M (1993) Isoproterenol antagonizes endothelial permeability induced by thrombin and thrombin receptor peptide. J Appl Physiol 75:1171–1179
Minnear FL, DeMichele MA, Moon DG, Rieder CL, Fenton JW 2nd (1989) Isoproterenol reduces thrombin-induced pulmonary endothelial permeability in vitro. Am J Physiol 257:H1613–1623
Kreienberg PB, Vincent PA, Bell DR, Saba TM, Minnear FL (1994) Isoproterenol decreases protein permeability in edematous isolated rabbit lungs: estimation of PS and sigma. J Appl Physiol 77:325–331
Berthiaume Y, Albertine KH, Grady M, Fick G, Matthay MA (1989) Protein clearance from the air spaces and lungs of unanesthetized sheep over 144 h. J Appl Physiol 67:1887–1897
Muscedere JG, Mullen JB, Gan K, Slutsky AS (1994) Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 149:1327–1334
Martynowicz MA, Walters BJ, Hubmayr RD (2001) Mechanisms of recruitment in oleic acid-injured lungs. J Appl Physiol 90:1744–1753
Bilek AM, Dee KC, Gaver DP 3rd (2003) Mechanisms of surface-tension-induced epithelial cell damage in a model of pulmonary airway reopening. J Appl Physiol 94:770–783
Dreyfuss D, Soler P, Saumon G (1992) Spontaneous resolution of pulmonary edema caused by short periods of cyclic overinflation. J Appl Physiol 72:2081–2089
Saldias FJ, Lecuona E, Comellas AP, Ridge KM, Rutschman DH, Sznajder JI (2000) beta-adrenergic stimulation restores rat lung ability to clear edema in ventilator-associated lung injury. Am J Respir Crit Care Med 162:282–287
Ottosson J, Svensjo E, Dawidson I, Persson T (1992) Septic shock in rats treated with terbutaline alone and in combination with chemotherapeutics, dexamethasone, and infusion of 3% albumin. Eur J Surg 158:89–93
Whitehurst VE, Joseph X, Alleva FR, Vick JA, Whittaker P, Zhang J, Fry BE Jr., Balazs T (1994) Enhancement of acute myocardial lesions by asthma drugs in rats. Toxicol Pathol 22:72–76
Effros RM (2006) The beta-agonist lung injury trial (BALTI). Am J Respir Crit Care Med 173:1290; author reply 1291–1292
Saumon G, Basset G, Bouchonnet F, Crone C (1987) cAMP and beta-adrenergic stimulation of rat alveolar epithelium. Effects on fluid absorption and paracellular permeability. Pflugers Arch 410:464–470
Berthiaume Y, Folkesson HG, Matthay MA (2002) Lung edema clearance: 20 years of progress: invited review: alveolar edema fluid clearance in the injured lung. J Appl Physiol 93:2207–2213
Matthay MA, Abraham E (2006) Beta-adrenergic agonist therapy as a potential treatment for acute lung injury. Am J Respir Crit Care Med 173:254–255
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant from CARDIF (Comité pour l'Assistance Respiratoire à Domicile d'Ile de France)
Part of this study was presented in abstract form at the 35th meeting of the SRLF (Société de Réanimation de Langue Française), 2007.
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0966-7.
Rights and permissions
About this article
Cite this article
de Prost, N., Dreyfuss, D., Ricard, JD. et al. Terbutaline lessens protein fluxes across the alveolo-capillary barrier during high-volume ventilation. Intensive Care Med 34, 763–770 (2008). https://doi.org/10.1007/s00134-007-0954-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0954-y