Abstract
Atherosclerosis was once thought to be solely a disease of lipid accumulation in the vessel wall. It does involve lipid accumulation, but inflammation appears to be an important driving factor. Consequently, our laboratory undertook to examine the role(s) of TLRs, and especially TLR2, in murine models of atherosclerosis.
Similar content being viewed by others
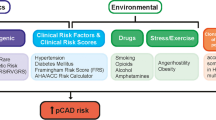
Atherosclerosis was once thought to be a simple lipid storage disease which caused pathology by arterial obstruction. It certainly leads to arterial obstruction, but not simply by accumulation of lipid. Now, it is clear that atherosclerotic lesions are foci of vessel wall inflammation [1–4]. Lesions begin very early in life as fatty streaks, progressing to pathological lesions under the influence of both genetic and lifestyle insults [5]. The final obstructive event is more likely to be a sudden thrombotic event rather than a slow, inexorable constriction by accumulation of lipid. During the major part of a human lifetime that may elapse between fatty streak formation and overt disease, there will be many events that can accelerate lesion progression. Genetic diseases, notably hypercholesterolemias, lead to very severe disease [6]. Lifestyle choices which include smoking, obesity, and excessive quiescence can also make significant contributions to disease progression. Finally, inflammatory disease elsewhere in the body, ranging from periodontitis to autoimmune disease, can have an exacerbating influence as well [7–10]. However, the factors which promote atherosclerotic lesion development do not do so uniformly throughout the arterial tree. Lesions form first at sites of disturbed flow [11]. Such sites are at vessel bifurcations and at the lesser curvature of the aortic arch. These sites display an inflamed phenotype even in the absence of any of the exacerbating disease factors. This is due to the altered flow patterns at these sites and the endothelial cell’s response to this disturbed flow [12–14]. Although the biochemical mechanisms by which endothelial cells detect flow patterns are beginning to be understood [15–17], the need to detect flow patterns is not. Evolutionarily, TLR expression and inflammation are certainly driven in part by infectious diseases [18]. However, no particular disease risk has been identified that would promote a pro-inflammatory phenotype only at arterial bifurcations and the lesser curvature of the aortic arch.
If inflammation is a hallmark of the disease, then it is only logical to study the roles of Toll-like receptors (TLRs) in atherosclerosis. TLRs are initiators of inflammation driven by agonists which may be either endogenous, such as sterile tissue damage [19], or exogenous, such as pathogens. Probably, given the vicissitudes of daily life, TLRs normally initiate inflammatory responses everyday. The majority of these are no doubt beneficial, promoting healing and homeostasis, but occasionally, they go awry and cause pathology. Atherosclerosis is one of the pathologic consequences, although TLRs are by no means the only cause or promoter of this disease.
Our laboratory studies TLRs and atherosclerosis in C57Bl/6J mice. There are two C57Bl/6J models in common use, each involving a single gene deletion that leads to plasma hypercholesterolemia. When wild-type C57Bl/6J mice are fed a high-fat, high-cholesterol diet, they do not develop atherosclerosis because they do not develop hypercholesterolemia. However, mice deficient in the gene encoding the low-density lipoprotein receptor (LDLr), a gene the lack of which causes human familial hypercholesterolemia and whose discovery and study won the Nobel prize for Michael Brown and Joe Goldstein [20], leads to hypercholesterolemia because synthesis and dietary intake of fat continues, but clearance from the plasma for catabolism in the liver is lost. The plasma cholesterol accumulates in the intima of the arteries in foam cells and leads to lesion development [13]. The other common model for the study of murine atherosclerosis is the ApoE-deficient mouse. ApoE deficiency leads to atherosclerotic lesion development because its absence causes massive hypertriglyceridemia, again leading to foam cell formation. For study of the TLRs in atherosclerosis, we have used the LDLr-deficient (LDLr−/−) mouse exclusively [21, 22]. The reason for this is a disadvantage of the ApoE model. Bone-marrow-derived cells (BMDC) synthesize and secrete significant quantities of ApoE. Thus, transplantating BMDC from ApoE-expressing mice into ApoE-deficient mice reverses the ApoE deficiency and the phenotype of the host mouse. However, transplanting bone marrow from an LDLr-expressing mouse into an LDLr−/− mouse does not reverse the phenotype of the host mouse [23]. The utility of these BMDC chimeras will become obvious below.
In addition to our experiments, reviewed below, others have studied disease development in MyD88-, TLR4-, and CD14-deficient mice [24, 25]. These studies showed that TLR4 and MyD88 deficiency lessened disease development, while CD14 deficiency had no effect on disease development.
We focused on TLR2 because in vitro experiments with human coronary artery endothelial cells showed that cells exposed to disturbed flow culture conditions to simulate flow patterns at sites of lesion development upregulated responsiveness to TLR2 agonists [26]. We found this to be due to an enhanced expression of TLR2 in response to disturbed flow. We did not observe that disturbed flow or no flow enhanced responses to TLR4 or TNF receptor ligands (see Fig. 1).
Initial results with LDLr−/−TLR2−/− mice showed that whole body deficiency of TLR2 results in decreased lesion burden after 10 or 14 weeks of high-fat diet consumption (see Fig. 2) [21]. Thus, functional TLR2 promotes disease. In these experiments, no agonist of TLR2 was deliberately administered to the mice, and thus, we refer to the TLR2 agonists involved as “endogenous” agonists. It should be understood that the mice studied were healthy, but not germ-free. Thus, the endogenous agonist may come from the genome of a commensal organism [27] or from the genome of the mouse itself. However, Wright et al. [28] have shown that germ-free ApoE-deficient mice do develop atherosclerosis, and thus, we favor the hypothesis that the endogenous TLR2 agonists are derived from the mouse itself. Others had shown previously that administration of exogenous LPS, the TLR4 agonist, promoted disease in rabbits and mice [29, 30]. In additional experiments, we showed that administration of Pam3CSKKKK, a synthetic TLR2 agonist, promoted additional disease in the LDLr−/− model and that this was abrogated in LDLr−/−TLR2−/− mice [21]. Thus, both endogenous and exogenous agonists promote disease by activation of TLR2 signaling, and TLR2 is one route for both the genetic and inflammatory pathways to atherosclerotic disease. These findings were recently confirmed in ApoE-deficient mice [31].
The technique of bone marrow transplantation allowed us to ask whether TLR2 expressed by BMDC or non-BMDC was disease-promoting. To our surprise, we found that BMDC and non-BMDC were both disease-promoting, but which cells were involved depended on whether the agonist was endogenous or exogenous. Non-BMDC-expressed TLR2 was sufficient to promote disease in response to the endogenous agonists, while BMDC-expressed TLR2 was sufficient to promote disease only in response to exogenous agonists (see Fig. 3) [21]. Given the known role of endothelial cells in regulating transport into the intima, it seems likely that the non-BMDC responding to endogenous TLR2 agonists are endothelial cells. Similarly, given the known relevance of monocytes or macrophages in responding to exogenous TLR2 agonists, it seems likely that these are the cells driving lesion development in response to the exogenous agonists.
The mechanism by which these specificities for endogenous and exogenous agonists come about is unknown. In this volume, Lee and Raz describe the differential effects of TLR9 expression in intestinal epithelial cells when TLR9 is expressed apically as opposed to basolaterally. In a similar vein, the work reported by Gewirtz notes that TLR5 is expressed only basolaterally in intestinal epithelial cells. We hypothesize that something similar could be happening with TLR2 on vascular endothelial cells that might explain our findings. Thus, if TLR2 were expressed by endothelial cells not at the apical membrane facing the vascular lumen but only at the basolateral membrane exposed to the intima, it would seem to be correctly located to detect endogenous agonists in the intima, but not available to detect exogenous blood-borne agonists. At present, there are no data to show where TLR2 is expressed in vascular endothelial cells, but endothelial cells are well known to express other proteins in a polarized fashion (e.g. [32]).
Using confocal microscopy of aortic arch tissue fragments, we have examined the distribution of TLR2 expression on the luminal face of the murine aortic arch (Fig. 4) [33]. These images show very little TLR2 expression in either wild-type C57Bl/6J mice or in LDLr−/− mice fed a chow diet. Importantly, even the minimal TLR2 expression that is present is seen in the lesser curvature region. Within 1 to 2 weeks of feeding a high-fat diet to LDLr−/− mice, TLR2 expression is significantly increased in the lesser curvature region of the aorta. However, it is expressed only by the endothelial cells, and not by the myeloid cells, in the intimal layer just below the endothelial cells [33]. Why these myeloid cells are not expressing TLR2 is open to conjecture. Brunn et al. [34] have shown that TLR4 signaling is strongly inhibited by extracellular matrix components. Something similar could be happening with TLR2. Certainly, the intimal macrophages are residing in a space containing much extracellular matrix material. Further, when one studies which cells are accumulating lipid at these early stages of lesion development, it is not the myeloid CD68-expressing cells, but rather the CD31-expressing endothelial cells [33]).
LDLr−/− and LDLr−/−TLR2−/− mice were fed a high-fat diet for the number of weeks as indicated in the figure. After sacrifice, expression of TLR2 and CD31, an endothelial cell membrane marker was visualized by laser scanning confocal microscopy. The figure shows that alterations in TLR2 expression and endothelial morphology are visible in LDLr−/− mice as early as one week after initiation of the diet. The LDLr−/−TLR2−/− mice show no staining for TLR2, as expected, and much less perturbation of endothelial morphology
A recent study concluded that overexpression of endothelial TLR2 in rabbits fed a high-fat diet led to enhanced progression of atherosclerosis. Thus, both diminution and enhancement of TLR2 have effects that point to a role for TLR2 in atherosclerosis [35].
What are the endogenous TLR2 agonists to which endothelial cells are sensitive ? Given the important role of oxidized lipoproteins in lesion development, it is tempting to point to these moieties, but no oxidized lipoprotein has yet been shown to be a TLR2 agonist. Other possibilities include HMGB1, biglycan, hyaluronic acid fragments, and SAA [19, 36–40]. All of these have been shown to be TLR2 agonists in vitro. We hypothesize that these agonists, and possibly others, may activate endothelial cells at lesion prone sites through TLR2 because it is only the endothelial cells that express TLR2.
If the aortic bone-marrow-derived myeloid cells do not express TLR2, how is it that exogenous agonists such as Pam3CSKKKK promote lesion development? There are at least two possibilities which we are considering. First, that the exogenously administered agonist stimulates a mediator response which drives TLR2 expression on the intimal myeloid cells within the intima. Alternatively, the exogenous agonist stimulates mediators that promote lesion-prone site-specific endothelial activation, which in turn serves to promote recruitment of monocytes that then enter the lesion and become activated by other means. These two hypotheses should not be difficult to distinguish experimentally.
In as much as inflammation is a hallmark of atherosclerosis, anti-inflammatory therapies will probably become more important as therapeutic measures. Statins are thought to have important anti-inflammatory properties, although their particular targets are not well defined [41]. Inhibitors of TLRs have not been tested in models of atherosclerosis, but there are some which should be tested. Youn et al. [42, 43] have found that curcumin and auranofin inhibit TLR4 by interfering with TLR4 homodimerization. Others have found that endotoxin analogs are also effective inhibitors of TLR4 [44, 45]. These reagents all interact with the extracellular domains of TLR4. We have recently utilized an high throughput screening assay to identify a group of low molecular weight, water-soluble reagents that interfere with the intracellular signal initiating mechanism of TLRs 2 and 4 [46]. Any of these approaches could lead to the development of important new drugs to modify the activity of TLRs.
In conclusion, there are abundant data to indicate that inflammatory processes play a pivotal role throughout the development of atherosclerosis. The idea that TLRs participate in these processes is now valid, although only two, TLR2 and TLR4, have been specifically shown to do so. Multiple cell types within the atheroma, including endothelial cells, dendritic cells, macrophages, vascular smooth muscle cells, and perhaps even adventitial fibroblasts, could participate in this inflammatory response. TLR2 does not cause atherosclerosis, but it certainly participates in its development. Given that the endogenous agonists that drive atherosclerotic disease are likely to be involved in normal surveillance and homeostatic processes, atherosclerosis can be considered as an innate autoimmune disorder.
References
Lusis AJ (2000) Atherosclerosis. Nature 407:233–241
Ross R (1999) Atherosclerosis—an inflammatory disease. N Engl J Med 340:115–126
Jongstra-Bilen J, Haidari M, Zhu SN, Chen M, Guha D, Cybulsky MI (2006) Low-grade chronic inflammation in regions of the normal mouse arterial intima predisposed to atherosclerosis. J Exp Med 203:2073–2083
Blankenberg S, Yusuf S (2006) The inflammatory hypothesis: any progress in risk stratification and therapeutic targets? Circulation 114:1557–1560
Zieske AW, Malcom GT, Strong JP (2002) Natural history and risk factors of atherosclerosis in children and youth: the PDAY Study. Pediatr Pathol Mol Med 21:213–237
Soutar AK, Naoumova RP (2007) Mechanisms of disease: genetic causes of familial hypercholesterolemia. Nat Clin Pract Cardiovasc Med 4:214–225
Van Doornum S, McColl G, Wicks IP (2002) Accelerated atherosclerosis: an extraarticular feature of rheumatoid arthritis? Arthritis Rheum 46:862–873
Triantafilou M, Gamper FGJ, Haston RM, Mouratis MA, Morath S, Hartung T, Triantafilou K (2006) Membrane sorting of Toll-like receptor (TLR)-2/6 and TLR2/1 heterodimers at the cell surface determines heterotypic associations with CD36 and intracellular targeting. J Biol Chem 281:31002–31011
Cao F, Castrillo A, Tontonoz P, Re F, Byrne GI (2007) Chlamydia pneumoniae-induced macrophage foam cell formation is mediated by Toll-like receptor 2. Infect Immun 75:753–759
Hauer AD, de Vos P, Peterse N, ten Cate H, van Berkel TJ, Stassen FR, Kuiper J (2006) Delivery of Chlamydia pneumoniae to the vessel wall aggravates atherosclerosis in LDLr−/− mice. Cardiovasc Res 69:280–288
Wasserman SM, Topper JN (2004) Adaptation of the endothelium to fluid flow: in vitro analyses of gene expression and in vivo implications. Vasc Med 9:35–45
Matharu NM, Rainger GE, Vohra R, Nash GB (2006) Effects of disturbed flow on endothelial cell function: pathogenic implications of modified leukocyte recruitment. Biorheology 43:31–44
Cunningham KS, Gotlieb AI (2005) The role of shear stress in the pathogenesis of atherosclerosis. Lab Invest 85:9–23
Dai G, Kaazempur-Mofrad MR, Natarajan S, Zhang Y, Vaughn S, Blackman BR, Kamm RD, Garcia-Cardena G, Gimbrone MA Jr (2004) Distinct endothelial phenotypes evoked by arterial waveforms derived from atherosclerosis-susceptible and -resistant regions of human vasculature. Proc Natl Acad Sci U S A 101:14871–14876
Tzima E, Irani-Tehrani M, Kiosses WB, Dejana E, Schultz DA, Engelhardt B, Cao G, DeLisser H, Schwartz MA (2005) A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature 437:426–431
Parmar KM, Larman HB, Dai G, Zhang Y, Wang ET, Moorthy SN, Kratz JR, Lin Z, Jain MK, Gimbrone MA Jr et al (2006) Integration of flow-dependent endothelial phenotypes by Kruppel-like factor 2. J Clin Invest 116:49–58
Dai G, Vaughn S, Zhang Y, Wang ET, Garcia-Cardena G, Gimbrone MA Jr (2007) Biomechanical forces in atherosclerosis-resistant vascular regions regulate endothelial redox balance via phosphoinositol 3-kinase/Akt-dependent activation of Nrf2. Circ Res 101:723–733
Ferwerda G, Girardin SE, Kullberg BJ, Le BL, de Jong DJ, Langenberg DM, van CR, Adema GJ, Ottenhoff TH, Van der Meer JW et al (2005) NOD2 and Toll-like receptors are nonredundant recognition systems of Mycobacterium tuberculosis. PLoS Pathog 1:279–285
Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, Prestwich GD, Mascarenhas MM, Garg HG, Quinn DA et al (2005) Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nat Med 11:1173–1179
Ishibashi S, Brown MS, Goldstein JL, Gerard RD, Hammer RE, Herz J (1993) Hypercholesterolemia in low density lipoprotein receptor knockout mice and its reversal by adenovirus-mediated gene delivery. J Clin Invest 92:883–893
Mullick AE, Tobias PS, Curtiss LK (2005) Modulation of atherosclerosis in mice by Toll-like receptor 2. J Clin Invest 115:3149–3156
Mullick AE, Tobias PS, Curtiss LK (2006) Toll-like receptors and atherosclerosis: key contributors in disease and health? Immunol Res 34:193–209
Boisvert WA, Spangenberg J, Curtiss LK (1995) Treatment of severe hypercholesterolemia in apolipoprotein E-deficient mice by bone marrow transplantation. J Clin Invest 96:1118–1124
Bjorkbacka H, Kunjathoor VV, Moore KJ, Koehn S, Ordija CM, Lee MA, Means T, Halmen K, Luster AD, Golenbock DT et al (2004) Reduced atherosclerosis in MyD88-null mice links elevated serum cholesterol levels to activation of innate immunity signaling pathways. Nat Med 10:416–421
Michelsen KS, Wong MH, Shah PK, Zhang W, Yano J, Doherty TM, Akira S, Rajavashisth TB, Arditi M (2004) Lack of Toll-like receptor 4 or myeloid differentiation factor 88 reduces atherosclerosis and alters plaque phenotype in mice deficient in apolipoprotein E. Proc Natl Acad Sci U S A 101:10679–10684
Dunzendorfer S, Lee HK, Tobias PS (2004) Flow-dependent regulation of endothelial Toll-like receptor 2 expression through inhibition of SP1 activity. Circ Res 95:684–691
Nijhuis MM, van der Graaf Y, Melief M-J, Schoneveld AH, de Kleijn DP, Laman JD, Pasterkamp G (2004) IgM antibody level against proinflammatory bacterial peptidoglycan is inversely correlated with extent of atherosclerotic disease. Atherosclerosis 173:245–251
Wright SD, Burton C, Hernandez M, Hassing H, Montenegro J, Mundt S, Patel S, Card DJ, Hermanowski-Vosatka A, Bergstrom JD et al (2000) Infectious agents are not necessary for murine atherogenesis. J Exp Med 191:1437–1442
Ostos MA, Recalde D, Zakin MM, Scott-Algara D (2002) Implication of natural killer T cells in atherosclerosis development during a LPS-induced chronic inflammation. FEBS Lett 519:23–29
Lehr HA, Sagban TA, Ihling C, Zahringer U, Hungerer KD, Blumrich M, Reifenberg K, Bhakdi S (2001) Immunopathogenesis of atherosclerosis: endotoxin accelerates atherosclerosis in rabbits on hypercholesterolemic diet. Circulation 104:914–920
Liu X, Ukai T, Yumoto H, Davey M, Goswami S, Gibson FC III, Genco CA (2007) Toll-like receptor 2 plays a critical role in the progression of atherosclerosis that is independent of dietary lipids. Atherosclerosis (in press)
Katsumi A, Orr AW, Tzima E, Schwartz MA (2004) Integrins in mechanotransduction. J Biol Chem 279:12001–12004
Mullick AE, Soldau K, Kiosses WB, Bell TA, Tobias PS, Curtiss LK (2007) Increased endothelial expression of Toll-like receptor 2 at sites of disturbed blood flow exacerbates early atherogenic events. J Exp Med, in press
Brunn GJ, Bungum MK, Johnson GB, Platt JL (2005) Conditional signaling by Toll-like receptor 4. FASEB J 19:872–874
Shinohara M, Hirata Ki, Yamashita T, Takaya T, Sasaki N, Shiraki R, Ueyama T, Emoto N, Inoue N, Yokoyama M et al (2007) Local overexpression of Toll-like receptors at the vessel wall induces atherosclerotic lesion formation. Synergism of TLR2 and TLR4. Arterioscler Thromb Vasc Biol 27:2384–2391
Park JS, Gamboni-Robertson F, He Q, Svetkauskaite D, Kim JY, Strassheim D, Sohn JW, Yamada S, Maruyama I, Banerjee A et al (2005) High mobility group BOx 1 protein (HMGB1) interacts with multiple toll like receptors. Am J Physiol Cell Physiol 290:C917–C924
Schaefer L, Babelova A, Kiss E, Hausser HJ, Baliova M, Krzyzankova M, Marsche G, Young MF, Mihalik D, Gotte M et al (2005) The matrix component biglycan is proinflammatory and signals through Toll-like receptors 4 and 2 in macrophages. J Clin Invest 115:2223–2233
Termeer C, Benedix F, Sleeman J, Fieber C, Voith U, Ahrens T, Miyake K, Freudenberg M, Galanos C, Simon JC (2002) Oligosaccharides of hyaluronan activate dendritic cells via Toll-like receptor 4. J Exp Med 195:99–111
Li M, Carpio DF, Zheng Y, Bruzzo P, Singh V, Ouaaz F, Medzhitov RM, Beg AA (2001) An essential role of the NF-kappa B/Toll-like receptor pathway in induction of inflammatory and tissue-repair gene expression by necrotic cells. J Immunol 166:7128–7135
Cheng N, He R, Ye RD (2007) 7 A.D. Serum amyloid A is an endogenous ligand for Toll-like receptor 2. Arterioscler Thromb Vasc Biol, abstract book: 23–24 (abstract)
Jain MK, Ridker PM (2005) Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov 4:977–987
Youn HS, Saitoh SI, Miyake K, Hwang DH (2006) Inhibition of homodimerization of Toll-like receptor 4 by curcumin. Biochem Pharmacol 72:62–69
Youn HS, Lee JY, Saitoh SI, Miyake K, Hwang DH (2006) Auranofin, as an anti-rheumatic gold compound, suppresses LPS-induced homodimerization of TLR4. Biochem Biophys Res Commun 350:866–871
Fort MM, Mozaffarian A, Stover AG, Correia JS, Johnson DA, Crane RT, Ulevitch RJ, Persing DH, Bielefeldt-Ohmann H, Probst P et al (2005) A synthetic TLR4 antagonist has anti-inflammatory effects in two murine models of inflammatory bowel disease. J Immunol 174:6416–6423
Shiozaki M, Iwano Y, Doi H, Tanaka D, Shimozato T, Kurakata S (2006) Syntheses of glucose derivatives of E5564-related compounds and their LPS-antagonistic activities. Carbohydr Res 341:811–822
Lee HK, Brown SJ, Rosen H, Tobias PS (2007) Application of beta-lactamase enzyme complementation to the high-throughput screening of Toll-like receptor signaling inhibitors. Mol Pharmacol 72:868–875
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tobias, P.S., Curtiss, L.K. TLR2 in murine atherosclerosis. Semin Immunopathol 30, 23–27 (2008). https://doi.org/10.1007/s00281-007-0102-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-007-0102-3