Abstract
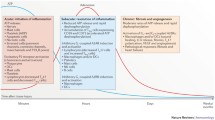
This review article provides a historical perspective on the role of purinergic signalling in the regulation of various subsets of immune cells from early discoveries to current understanding. It is now recognised that adenosine 5′-triphosphate (ATP) and other nucleotides are released from cells following stress or injury. They can act on virtually all subsets of immune cells through a spectrum of P2X ligand-gated ion channels and G protein-coupled P2Y receptors. Furthermore, ATP is rapidly degraded into adenosine by ectonucleotidases such as CD39 and CD73, and adenosine exerts additional regulatory effects through its own receptors. The resulting effect ranges from stimulation to tolerance depending on the amount and time courses of nucleotides released, and the balance between ATP and adenosine. This review identifies the various receptors involved in the different subsets of immune cells and their effects on the function of these cells.
Similar content being viewed by others
Synopsis
ᅟ
Introduction
ᅟ
Purinergic signalling in the main subsets of immune cells
Polymorphonuclear leukocytes
Neutrophils
Eosinophils
Basophils
Mast cells
Section summary
Monocytes, macrophages and microglia
Monocytes
Macrophages
Microglia
Section summary
Dendritic cells
P1 receptors
P2 receptors
Section summary
Lymphocytes
T and B lymphocytes
Natural killer (NK and NKT) cells
Section summary
Concluding remarks
ᅟ
Introduction
Although nucleotides, such as adenosine 5′-triphosphate (ATP) and uridine 5′-triphosphate (UTP), are mainly intracellular, they are released into the extracellular fluids by various mechanisms. One of them is cell damage and death: both necrotic and apoptotic cells release ATP and other nucleotides that thus constitute “danger signals” or damage associated molecular pattern [1–3]. In the absence of cell death, they are also released in response to various types of stress: mechanical stimulation (stretch, shear stress) [4], hypoxia or pathogen invasion [5, 6]. Specific mechanisms of release include: exocytosis of secretory granules, vesicular transport [7, 8] and membrane channels, such as ATP-binding cassette transporters, pannexins [9–11] and connexins [12]. In particular, nucleotides are released by exocytosis during platelet aggregation and synaptic transmission. For many years, cells of the immune system were not considered to be innervated, but there is increasing recognition that nerves can influence the immune system and the field of neuroimmunology is growing rapidly [13–15].
Once in the extracellular fluids, nucleotides are rapidly degraded by a variety of ectonucleotidases [16], such as the ENTPDases, like CD39 that degrades ATP into adenosine 5′-diphosphate (ADP) and ADP into adenosine monophosphate (AMP) and CD73/5′-nucleotidase that converts AMP into adenosine. Receptors for extracellular nucleotides and their degradation products such as adenosine have been progressively characterized. Subdivision of purinergic receptors between P1 (adenosine) and P2 (ATP, ADP) was proposed by Burnstock in 1978 [17]. A further subdivision of P2 receptors between P2Y and P2X was made in 1985 [18]. It is now well established that signalling by extracellular nucleotides is mediated by these two families of receptors, the molecular structure of which has been characterized: P2Y receptors are metabotropic G protein-coupled while P2X receptors are oligomeric ion channels.
Numerous reviews on various aspects of purinergic signalling in the immune system are available (Table 1). In the history and development of knowledge about purinergic signalling, early workers focussed on adenosine, while those concerned with ATP rarely referred to adenosine. This is obviously an inadequate approach since the effects of ATP and adenosine, its breakdown product that is rapidly produced by ectonucleotidases, are intimately related. In this review, purinergic signalling in immune cells will be covered in a comprehensive and historical way, following the increase in knowledge from the early discoveries to current understanding. The review will consider the major subsets of immune cells and, for each of them, address the mechanisms of nucleotides release and adenosine generation, as well as the repertoire of functional P1 and P2 receptors that they express.
Purinergic signalling in the main subsets of immune cells
Polymorphonuclear leukocytes
Neutrophils
P1 receptors
Ectoenzymes that hydrolyse ATP have been observed on guinea pig polymorphonuclear leukocytes [19–21]. In particular, both CD39 and CD73 ectonucleotidases are present on neutrophil membranes [22]. Furthermore, neutrophils express mRNA for A1, A2A, A2B and A3 receptors [23], but the mRNA for A2A and A3 receptors are the most abundant [24]. Adenosine was shown to be a physiological modulator inhibiting the generation of superoxide (O2 −) anion by neutrophils via A2 receptors [25–29]. Not surprisingly, dipyridamole, which prevents the uptake of adenosine, thereby increasing extracellular levels, inhibits O2 − generation by neutrophils [30]. Adenosine also inhibited the degranulation induced by the chemotactic peptide N-formyl-methionyl-leucyl-phenylalanine (fMLP) [28], phagocytosis [31] and the bactericidal function of neutrophils [32]. It was proposed that the inhibitory actions of adenosine on neutrophils were due to calcium entry blockade [33–35]. Adenosine inhibited neutrophil respiratory bursts in association with an increase in cyclic AMP (cAMP) and reduction in [Ca2+]i [36, 37]. Occupancy of A2A receptors by adenosine inhibits fMLP-induced neutrophil activation via cAMP and protein kinase A regulated events [38]. Caffeine intake results in increase in cAMP accumulation and decrease in O2 − anion production in human neutrophils, mediated by A2A receptors [39]. Activation of A2A receptors also inhibited the expression and release of various cytokines and chemokines after lipopolysaccharide (LPS) stimulation of neutrophils [40]. But other studies showed that both the A2B and the A3 receptors can also play a role in these inhibitory actions. Tumour necrosis factor-α (TNF-α) production by neutrophils following renal ischemia-reperfusion was increased in A2B-deficient mice [41]. Activation of A2B receptors also inhibited fMLP-induced O2 − production [42]. The A3 receptor is also involved in the inhibition of O2 − production [43] and of degranulation [44]. Adenosine downregulated ligand-stimulated leukotriene B4 biosynthesis in neutrophil suspensions [45], but it potentiated neutrophil cyclooxygenase-2 via A2A receptors [46].
In contrast, there are discrepant reports concerning the action of adenosine on neutrophil chemotaxis. It was claimed in 1982 that adenosine had no effect on the chemotaxis of neutrophils, although it did enhance the inhibition of chemotaxis by 3-deaza-(±)aristeromycin [47]. However, it was reported later that adenosine promotes neutrophil chemotaxis [48], perhaps via A1 receptors [49]. It was shown recently that the recruitment of neutrophils and other leukocytes in the lung during influenza infection is reduced in A1-deficient mice [50]. In contrast, LPS-induced recruitment of neutrophils in the lung was increased in A2A-deficient mice and experiments with chimeric mice revealed that this involves a direct inhibitory effect of the A2A receptor in myeloid cells [51]. Similar results were obtained in A2B-deficient mice [52]. Interestingly, in A2A-deficient mice, neutrophils were increased in the alveolar space [51], whereas they were increased in the interstitium of A2B-deficient mice [52]. Chen et al. [24] showed that adenosine stimulates neutrophil migration and amplifies the action of chemotactic signals through A3 receptors that are recruited to the leading edge (see Fig. 1). In A3-deficient mice, the recruitment of neutrophils was reduced in the lung during sepsis [53] and in the colon after induction of colitis by dextran sulphate [54]. Interestingly neutrophil chemotaxis requires excitatory signals at the front and inhibitory signals at the back of cells. This inhibitory signal at the back might be mediated by adenosine acting on A2A receptors [55] (Fig. 1).
Proposed model of neutrophil chemotaxis. As previously reported, stimulation of chemoattractant receptors induces local release of ATP through PANX1 channels at the site that first encounters the chemoattractant. Autocrine feedback via P2Y2 receptors amplifies the chemotactic signal and triggers cell polarization, whereby cells assume an elongated shape, and PANX1, CD39 (NTPDase1) and A3 adenosine receptors accumulate at the leading edge. In the current study, we found that A2A receptors are translocated from the leading edge toward the back of polarized neutrophils and that inhibitory signaling via A2A receptor-dependent cAMP accumulation inhibits excitatory chemotactic signalling by blocking FPR-dependent ERK and p38 MAPK activation globally with the exception of the leading edge. ALP alkaline phosphatase, ADO adenosine, PIP3 phosphatidylinositol (3,4,5)-triphosphate. (Reproduced from [55], with permission from the American Society for Biochemistry and Molecular Biology)
There is evidence that adenosine can modulate the interaction of neutrophils with pathogens. A3 receptors aggregate in highly polarised immunomodulatory microdomains of human neutrophil membranes. They promote the formation of filipodia-like projections (cytonemes) that can extend up to 100 μm to tether pathogens. Exposure to bacteria or an A3 agonist stimulates the formation of these projections and bacterial phagocytosis, whereas an A3 antagonist inhibits cytoneme formation [56].
Neutrophil adherence to endothelium was enhanced via A1 receptors and inhibited via A2 receptors [57, 58]. It is now believed that adenosine generated from ATP by CD39 and CD73 on the vascular surface functions as an anti-adhesive signal for neutrophil binding to microvascular endothelia through activation of neutrophil adenosine A2A and A2B receptors [59]. Activation of A2A receptors also inhibits expression of α4/β1 integrin on human neutrophils [60]. Human neutrophils activated by fMLP increased the number of cell surface β2 integrins on endothelial cells and induced the shedding of L-selectin. These effects were inhibited by adenosine, most likely via the A2A receptor [61]. A2 receptor activation inhibited neutrophil injury to coronary endothelium [62]. Adenosine also acts on endothelial receptors, thereby promoting vascular barrier function, providing a mechanism to dampen vascular leak syndrome during neutrophil–endothelial interactions [63] and regulating neutrophil chemotaxis [64]. Exposure of human endothelial cells to hypoxia/re-oxygenation caused increased neutrophil adhesion, an effect prevented by adenosine [65]. Adenosine also reduced the stimulatory effect of neutrophils on tissue factor-dependent coagulant activity of endothelial cells as a result of the inhibition of neutrophil adhesion to endothelial cells mediated by A2 receptors [66].
Adenosine might also play a role in the regulation of neutrophil number. Synergistic effects of granulocyte colony-stimulating factor and dipyridamole increased neutrophil production in mice [67]. Both effects were inhibited by adenosine deaminase (ADA). Theophylline has an immunomodulatory action on neutrophil apoptosis via A2A receptor antagonism [68].
The expression of adenosine receptors on neutrophils can be modulated in pathological conditions and following various interventions. A2A receptors on freshly isolated human neutrophils are upregulated after stimulation by LPS or TNF-α, and this may represent a feedback mechanism to control inflammation [69]. A2B receptor activity in neutrophils is reduced in patients with systemic sclerosis [70]. A 4.6-fold decrease in adenosine-mediated inhibition of neutrophils from patients with septic shock was reported [71]. Hypertonic saline upregulates A3 receptor expression on activated neutrophils and increases acute lung injury after sepsis [72]. Alterations in the functional expression of both A2A and A3 receptors in human neutrophils treated with pulsing electromagnetic fields have been reported [73, 74].
P2 receptors
ATP induces an increase in [Ca2+]i in human [75] and mouse [76] neutrophils. ATP and UTP, acting via P2U (i.e. P2Y2 and/or P2Y4) receptors, coupled to the inositol 1,4,5-trisphosphate pathway and increased [Ca2+]i [37]. This was associated with a priming of neutrophils for enhanced O2 − generation when stimulated by other agonists [37, 77, 78]. The release of Ca2+ from thapsigargin-sensitive intracellular stores is essential for this nucleotide-induced priming in human neutrophils [79], indicating mediation via P2Y receptors. Enhanced O2 − responses of rat neutrophils stimulated by formyl chemotactic peptide were evoked by ATP and ADP, whereas adenosine and AMP were inhibitory [80–82]. ATP and UTP also stimulated granule secretion from human neutrophils [83, 84] and potentiated the secretion induced by chemotactic peptides [78]. They also induced neutrophil aggregation [78, 85].
Human neutrophils release ATP from the leading edge of the cell surface to amplify chemotaxic signals and direct cell orientation by feedback via P2Y2 receptors (Fig. 1) [24, 55, 86]. The importance of this mechanism in pathology is demonstrated by studies showing that the infiltration of neutrophils in the smoke-injured lung [87] and in the liver damaged by toxic agents [88] is decreased in P2Y2 knockout (−/−) mice. Chen et al. [24] also showed that neutrophil ectonucleotidases hydrolyze ATP to adenosine, which, via A3 receptors, also promoted cell migration (Fig. 1). In agreement with this concept, both P2Y2 and A3 receptors control the recruitment of neutrophils to the lungs in a mouse model of sepsis [53]. Neutrophil chemotaxis requires excitatory signals at the front and inhibitory signals at the back of cells that regulate cell migration. P2Y2 receptors, as well as A3 receptors, were shown to contribute to excitatory signals at the front, while adenosine acting on A2A receptors contributed to the inhibitory signal at the back [55] (Fig. 1).
The P2Y14 receptor was shown to be functionally expressed on human neutrophils [89], and uridine-diphosphate (UDP)-sugars promoted Rho-mediated signalling and chemotaxis in human neutrophils [90], which was blocked by a P2Y14 antagonist [91].
Neutrophil apoptosis induced by ATP was inhibited by P2Y11 receptor activation, and it was suggested that targeting of P2Y11 receptors could retain the immune functions of neutrophils and reduce the injurious effects of increased neutrophil longevity during inflammation [92]. A later paper showed that P2Y11 receptors mediate ATP-enhanced chemotactic responses of rat neutrophils [93].
RT-PCR and Northern blot analysis revealed the presence of P2X7 receptors on neutrophils and 2′ (3′)-O-(4-benzoylbenzoyl) ATP (BzATP), a potent P2X7 receptor agonist, stimulated production of O2 − [23, 94]. A role of P2X7 in protection against neutrophil apoptosis has been reported [95, 96]. Neutrophil accumulation in the skin during croton oil-induced irritant contact dermatitis was reduced in P2X7-deficient mice [97]. However, it was claimed more recently that human neutrophils do not express P2X7 receptors [98]. In an RT-PCR study of human neutrophils, mRNA for P2X1 was strongly expressed, while mRNA for P2X4 and P2X5 was weakly expressed and P2X7 mRNA was not detected [99]. P2X1 receptors mediate neutrophil chemotaxis via Rho kinase activation [100]. A study using P2X1 receptor knockout mice led to the conclusion that P2X1 receptors play a protective role in endotoxaemia by negatively regulating systemic neutrophil activation, thereby limiting the oxidative response, coagulation, and organ damage [101].
Eosinophils
P1 receptors
A3 receptors were identified on human eosinophils and their activation led to increased [Ca2+]i [102]. However, the role of adenosine and A3 receptor signalling on this cell type remains controversial with both pro- and anti-inflammatory activities of adenosine being reported. Adenosine was shown to potentiate the production of O2 − by guinea pig pulmonary eosinophils [103]. However, an inhibition of degranulation and O2 − anion release from human eosinophils was observed later and shown to be mediated by A3 receptors [104]. In human eosinophils, adenosine inhibits chemotaxis via the A3 receptor [105, 106], whereas a stimulatory effect has been observed in eosinophils of ADA-deficient mice [107].
P2 receptors
Nucleotides were shown to stimulate human eosinophils, and it was suggested that since ATP is released from autonomic nerves and activated platelets, it could modulate the migration and other activities of eosinophils in vivo [76]. Thrombin-stimulated platelets secrete ATP, a chemotactic factor that attracts eosinophils [108]. ATP was shown to be a potent activator of eosinophils, suggesting a role for ATP in the pathogenesis of eosinophilic inflammation as an activator of pro-inflammatory effector functions [109]. Expression of P2Y1, P2Y2, P2Y4, P2Y6, P2Y11 and P2X1, P2X4, P2X5 and P2X7 receptor mRNA has been observed in human eosinophils (see Fig. 2) [99, 110]. It was also shown in this paper that purinoceptors mediate increase in [Ca2+]i and the production of reactive oxygen intermediates. The functional characterization of P2Y and P2X receptors on human eosinophils was undertaken, and it was shown that UTP and ATP had a greater stimulatory effect on the production of reactive oxygen metabolites, actin polymerization and chemotaxis than the selective P2X receptor agonists α,β-methylene ATP and BzATP, suggesting a predominant role of P2Y receptors [111]. However, P2Y and P2X agonists had similar effects regarding intracellular calcium transients and the adhesion molecule CD11b. In a study of human eosinophils, ATP was shown to trigger secretion of eosinophil cationic protein, probably via P2Y2 receptors, while ATP induced interleukin (IL)-8, probably via P2Y6, P2X1 and P2X7 receptors [112]. Autocrine release of ATP and P2 receptors, presumably P2Y2, were shown to play a pivotal role in human eosinophil degranulation and production of pro-inflammatory cytokines in response to the endogenous danger signal, crystalline uric acid [113]. Human eosinophils respond also to ADP via P2Y12 receptors to elicit eosinophil secretion of peroxidase [114]. The use of knockout mice has allowed us to demonstrate the crucial role of P2Y2 receptors in the accumulation of eosinophils in the lungs during allergic inflammation. This involves both a direct chemotactic effect of ATP mediated by the eosinophil P2Y2 receptor [115] and an indirect effect on endothelial cells, where ATP via P2Y2 stimulates the expression of VCAM-1 that mediates eosinophil adherence and infiltration, and its soluble form that is chemotactic for eosinophils [116].
P2 receptors expressed by human eosinophils. a P2Y receptors. b P2X receptors. (Reproduced from [110], with permission from Elsevier)
Basophils
P1 receptors
It was reported that human basophils have a receptor for adenosine that mediates inhibition of immunoglobulin (Ig)E-mediated histamine release [117, 118]. In later papers, it was shown that the inhibitory effect of adenosine is mediated by an A2 receptor and cAMP increase [119–121].
P2 receptors
Activation of permeabilised rat basophilic leukaemia cells (RBL-2H3) by adenosine-5′-O-(3-thio)triphosphate led to secretion of allergic and inflammatory mediators [122]. In a recent paper, it was shown that degranulation and histamine release from human basophils, associated with type 1 allergy, was evoked by UTP and particularly UDP, suggesting mediation by P2Y2 and/or P2Y4 and P2Y6 receptors [123].
Mast cells
P1 receptors
Potentiation of A23187 calcium ionophore-induced mast cell release of histamine by adenosine was initially reported [124]. Anti-IgE-induced release of histamine from mast cells was also enhanced by adenosine [125–130], as was β-hexosaminidase release from bone marrow-derived mast cells [131]. Histamine release from human adenoidal mast cells induced by concanavalin A or acetylcholine was also enhanced by adenosine [132]. Although other mechanisms have been proposed [133, 134], the potentiation of histamine release by adenosine appears to be mediated by A3 receptors, since it was mimicked by selective A3 agonists [135, 136] and abolished in A3-deficient mice [137]. Furthermore, it was shown that the increase of cutaneous vascular permeability and extravasation of plasma proteins in response to adenosine was abolished in mast cell-deficient mice as well as in A3-deficient mice [138]. Similarly, adenosine-induced bronchoconstriction was attenuated in mast cell-deficient and A3-deficient mice [139].
The response of human lung mast cells to adenosine was biphasic: low concentrations of adenosine potentiated release of histamine, while high concentrations elicited inhibition [140]. Adenosine also inhibited IgE-dependent degranulation of human skin mast cells via A2A receptors [141]. Both A2A and A2B receptors were identified on mouse bone marrow-derived mast cells [142]. Using knockout mice, it was demonstrated that the inhibition of mast cell degranulation by adenosine in mediated by the A2B receptor, while the combined action of A2B and A2A receptors is responsible for the inhibition of cytokine production [143]. However, the role of adenosine receptors in mast cell regulation is more complex, since the stimulatory effect of adenosine on the release of angiogenic factors such as vascular endothelial growth factor (VEGF) was shown to involve a cooperation between A2B and A3 receptors [144, 145]. Furthermore, in umbilical cord blood-derived mast cells, IL-4 increased the potentiating effect of adenosine on degranulation via an upregulation of A2B receptors, whereas these receptors were shown previously to be inhibitory in murine mast cells [146].
P2 receptors
ATP was reported early to evoke calcium-dependent histamine release with degranulation of rat mast cells [147–152]. It was suggested that the source of ATP may be innervating nerve fibres [153, 154], as discussed below. A correlation was shown between the ATP levels in rat peritoneal mast cells and histamine released by the anaphylactic reaction and compound 48/80 [155, 156]. ATP was shown to induce cytokine expression and apoptosis via P2X7 receptors on murine mast cells [157], supporting the earlier recognition of ATP-induced pore formation in rat peritoneal mast cells [158]. Interestingly, colitis was improved in mast cell-deficient mice as well as in those mice reconstituted with P2X7 −/− mast cells, showing the role of mast cell activation by ATP via the P2X7 receptor in intestinal inflammation [159]. ATP-induced cytokine and chemokine expression could also be mediated by P2X1 and P2X3 receptors on murine mast cells [160]. Functional expression of P2X1, P2X4 and P2X7 receptors in human lung mast cells was presented [161]. Mast cells are a major source of protein arginine deiminase, and it was shown that ATP induced protein arginine deiminase 2-dependent citrullination in mast cells via P2X7 receptors [162].
G protein-coupled P2Y receptors were also shown to mediate mast cell activation [163, 164]. UDP-glucose acting via P2Y14 receptors was shown to be a mediator of mast cell degranulation and considered as a potential therapeutic target for allergic conditions [165]. In a recent paper, all P2Y receptor subtypes were shown to be expressed in variable levels by human LAD2 mast cells [166]. Although P2Y4 and P2Y11 receptors were highly expressed, they did not appear to play a major role in degranulation, whereas P2Y14 receptors did.
Autonomic nerves as well as sensory-motor nerves innervate immune cells and release ATP as a cotransmitter in close vicinity of immune cells [167]. Indeed in accordance with the definition of the autonomic neuroeffector junction, close contact of nerve varicosities with effector cells in effect constitutes innervation, albeit of a transient nature [168, 169]. Mast cells were the first claimed to be innervated [170]. Antidromic stimulation of sensory nerves increased degranulation of mast cells in the skin, and this effect was mimicked by ATP [171]. Close opposition of nerve varicosities containing small and large vesicles and mast cells in the mucosa of intestine was shown with electron microscopy [154, 172] and also in cerebral blood vessels [173] (Fig. 3). Synovial mast cell activity that contributes to inflammation in joints was shown to be influenced by both unmyelinated afferent and sympathetic efferent nerves [174]. Sympathetic and trigeminal sensory nerve fibres influence rat dural mast cells and have been shown to play a role in the pathophysiology of vascular headache [175]. Functional interactions between sensory nerves and mast cells of the dura mater have been described in both normal and in inflammatory conditions [176]. Vagus nerve stimulation modulates histamine content in mast cells in the rat jejunal mucosa [177]. From a study of co-cultures of nerves and mast cells, it was concluded that ATP released from activated mast cells was an important mediator to activate nerves [178, 179]. While substance P released from nerves activated mast cells, ATP released from mast cells in response to anti-IgE antibody activated superior cervical ganglia neurons. Few investigations have been carried out about the influence of nerves on non-mast cell immune cells, but evidence has been presented that nerve fibres form close relationships with other immune cells, such as eosinophils [180], macrophages [181], and T and B lymphocytes [182–184].
a Close apposition between rat mast cell protease 1 immunoreactive and calcitonin gene-related peptide immunoreactive nerve fibres observed by confocal microscopy. b Ultrathin section of rabbit middle cerebral artery showing granular cells (G) separated by a distance of less than 200 nm. V varicosities; arrowheads basement membranes. Magnification, ×29374. (a Reproduced from [176] and b from [173], with permission from Elsevier)
Section summary
Adenosine and ATP have opposite effects on O2 − generation and other functions of neutrophils: adenosine has an inhibitory effect, mediated mainly by A2A and A2B receptors, while ATP has a potentiating effect. On the other hand, ATP and adenosine cooperate to amplify the migration of neutrophils induced by chemotactic signals: this involves a stimulatory effect mediated by P2Y2 and A3 receptors expressed at the front of the neutrophils and an inhibitory effect of A2A receptors expressed at the back of the cells.
ATP via P2Y2 receptors also plays an important role in the migration of eosinophils and their accumulation in the lungs during allergic inflammation. Adenosine exerts a dual effect on mast cell degranulation: stimulation through A3 receptors and inhibition via A2A and A2B receptors.
Monocytes, macrophages and microglia
Monocytes
P1 receptors
Adenosine was initially reported to inhibit the production of the second complement component (C2) of human monocytes [185], and this effect was later shown to be mediated by A2 receptors [186]. Subsequently, it was also shown that A1 receptors were expressed on cultured human monocytes and rheumatoid synovial fluid mononuclear phagocytes [187]. Enhancement of Fcγ receptor-mediated phagocytosis was induced via A1 receptors, while A2 receptors mediated reduction of Fcγ phagocytosis in cultured monocytes. TNF-α production in human monocytes was inhibited by P1 receptor agonists [188]. Both A2A and A2B receptors were shown to be involved in the inhibition of TNF-α production [189]. Activation of A2A receptors also inhibited IL-12 and stimulated IL-10 production by human monocytes [190, 191]. These actions may contribute to suppression of Th1 responses. However, the effect of P1 receptor agonists on cytokine release from human mononuclear cells was shown to depend on the specific Toll-like receptor (TLR) subtype used for stimulation: the A2A agonist CGS21680 inhibited TLR4-mediated TNF-α release, but potentiated TLR3- and TLR5-mediated IL-6 release [192]. Activation of A2A receptors also inhibited LPS-induced IL-18 production, expression of adhesion molecules and production of TNF-α, in human monocytes [193, 194]. Activation of A1 receptors promoted multinucleated giant cell formation by human monocytes [195]. Adenosine analogues were shown to produce apoptosis of human mononuclear cells via A2A and A3 receptors [196].
P2 receptors
ATP and ADP were initially shown to increase [Ca2+]i in monocytes and to regulate the activity of adhesion receptors CD11b/CD18 [197]. ATP and ADP activated human promonocytic U-937 cells apparently via different P2 receptor subtypes [198]. mRNA for P2X7 and P2Y2 receptors was shown to be expressed by human THP-1 monocytic cells and monocytes, and the presence of these receptors was supported by pharmacological data [199–201]. P2X7 receptor expression in THP-1 monocytes was positively modulated by pro-inflammatory stimuli and negatively modulated by cAMP, a classic anti-inflammatory second messenger [202]. P2X7 receptors mediated ATP-induced IL-1β release from human and canine monocytes [203–205], an effect requiring priming by LPS [206]. This mechanism plays a major role in the physiological control of IL-1β secretion by monocytes. Indeed microbial components acting on different pathogen-sensing receptors, as well as the danger signals uric acid and C3a, induced the activation of human monocytes and their secretion of IL-1β and IL-18 through a process involving, as an initial event, the release of ATP [207–209]. This was followed by the autocrine stimulation of P2X7 receptors and inflammasome activation [210] (Fig. 4). Indeed, IL-1β secretion was inhibited by apyrase as well as by P2X7 antagonists. Additional evidence in favour of the involvement of P2X7 was the observation that the P2X7 receptor polymorphism Glu496Ala, which is associated with a loss of function, impaired ATP-induced IL-1β release from human monocytes [211].
Hypothetical sequence of events leading to P2X7 receptor and pannexin 1 (panx-1)-mediated inflammasome activation. Pathogen-associated molecular patterns (PAMPs) bind to Toll-like receptors (TLRs) and drive interleukin (IL)-1β gene expression and accumulation of the pro-cytokine. Extracellular ATP binds to the P2X7 receptor and triggers K+ efflux and panx-1 activation. The functional significance of K+ efflux is unknown, although it might facilitate or even precipitate inflammasome activation. Likewise, the mechanism of panx-1 activation by the P2X7 receptor is unknown. Panx-1 in turn activates the inflammasome. Data suggest that the ion-carrying activity of panx-1 is unnecessary for inflammasome activation. The activated inflammasome then cleaves pro-IL-1β. Thus, stimulation of the inflammasome by extracellular ATP can be split into two steps: (a) recruitment and activation of panx-1 by the P2X7 receptor and (b) activation of the inflammasome by panx-1. Colour coding: white PAMP, red TLR, green NALP3 inflammasome, orange protein–protein interaction domains, further subdivided into orange square, ASC apoptosis-associated speck-like protein containing a caspase-recruitment domain and orange octagon, pyrin domain; yellow FIIND domain, light blue caspase domain (Casp-1), dark blue biologically active IL-1β and IL-1β propiece, violet P2X7 receptor, light green panx-1. (Reproduced from [210], with permission from Elsevier)
ATP was initially described as a chemoattractant for monocytes [212, 213]. More recently apoptotic thymocytes were found to release nucleotides leading to the recruitment of monocytes [3]. This release is mediated by pannexin 1 channels, as demonstrated by the use of pharmacological inhibitors and small interfering RNA (siRNA), and involves the activation of pannexin 1 by caspases [9]. Monocyte recruitment by apoptotic cells supernatants, demonstrated inter alia in the murine air-pouch model, was decreased in P2Y2 −/− mice, leading to impaired clearance of the apoptotic cells. These data clearly identify ATP as a find-me signal acting through the P2Y2 receptor that recruits monocytes in order to clear apoptotic cells.
Other effects of extracellular nucleotides on monocytes include increased surface expression of Mac-1 integrin [214], secretion of IL-8 that might involve P2Y2 and P2Y6 receptors [215, 216], inhibition of soluble HLA-G secretion [217], secretion of VEGF [218] and modulation of phagocytosis [219]. These last 3 effects involve P2X7 receptors. In human monocytes, ATP was reported to increase cAMP via the P2Y11 receptor, and thereby to inhibit proinflammatory cytokines production and to increase the release of IL-10 [213].
Macrophages
P1 receptors
Chemotaxis and lysosomal secretion were shown to be inhibited by adenosine and analogues in the mouse macrophage cell line RAW 264 or murine peritoneal macrophages [220, 221]. Adenosine was reported to inhibit TNF-α expression, induced by LPS in the mouse macrophage cell lines J774.1 [222] and RAW264.7 [223], whereas it potentiated nitric oxide synthase (NOS) expression induced by LPS in RAW 264.7 mouse macrophages [224, 225]. Interferon (IFN)-γ upregulated A2B receptor expression in macrophages [226], while TNF-α or LPS induced A2A expression via nuclear factor-κB, as part of a feedback mechanism for macrophage deactivation [227, 228]. TNF-α release from macrophages was inhibited by adenosine via A2A and A2B receptors [229–232] and IL-10 production was augmented by adenosine acting through A2B [233] or A2A [234, 235] receptors. Interestingly, it was shown that pro-inflammatory macrophages (M1 cells that release TNF-α) have a low expression of ecto-nucleotidases and rate of ATP hydrolysis as compared to anti-inflammatory macrophages (M2 cells that release IL-10) [236]. A2A receptors also upregulated the expression of peroxisome proliferator-activated receptors [237] and hypoxia-inducible factor 1 [238]; this could contribute to the anti-inflammatory and tissue-protecting action of adenosine. A2A receptors mediated upregulation of vascular endothelial growth factor expression in murine [239] and human [240] macrophages. On the other hand, activation of A3 receptors stimulates matrix metalloproteinase-9 secretion by macrophages [241], and glucocorticoids promote survival of macrophages through stimulation of A3 receptors [242].
P2 receptors
Early reports showed that ATP permeabilised the plasma membrane to fluorescent dyes [243, 244], promoted cation fluxes [245–247], increased [Ca2+]i, induced a respiratory burst and O2 − generation [248, 249], inhibited phagocytosis [250] and induced cytotoxicity [251] and cell lysis [252] in a variety of macrophage populations. ATP was also shown to stimulate phosphoinositides hydrolysis and eicosanoid synthesis in mouse peritoneal macrophages [253]. Oxidized ATP (oxATP) was shown to irreversibly inhibit the permeabilization of the plasma membrane, but not the fast mobilization of Ca2+ induced by ATP in macrophages, supporting the expression of P2X7, then called P2Z, receptors in the J774 macrophage cell line [254]. P2X7 receptors were also shown to be expressed by BAC1.2F5 mouse macrophages, mediating both pore-forming and phospholipase (PL)-D activity [255], and in human monocyte-derived macrophages [256, 257].
Later studies demonstrated the involvement of the P2X7 receptor in several responses of macrophages to danger, in particular the proinflammatory response mediated by IL-1β secretion, bacterial killing and the associated macrophage death. ATP was shown to promote the maturation and release of IL-1β from macrophages [258, 259], via P2X7 receptors [260, 261]. ATP-induced secretion of IL-1β was abolished in macrophages from P2X7-deficient mice and involved inflammasome assembly and caspase-1 activation [262–264]. Activation of the inflammasome and release of IL-1β in macrophages dying through autophagy [265] or stimulated by serum amyloid A [266] involved the release of ATP and the activation of P2X7. P2X7 −/− mice showed increased survival after lung adenoviral infection, resulting from a decreased production of IL-1β by macrophages [264]. These mice were also protected against smoke-induced lung inflammation and emphysema, as a result of decreased activation of lung macrophages [267].
P2X7-mediated ATP-induced killing of mycobacteria by human macrophages was initially reported in 1997 [268]. This seminal observation was later confirmed in numerous studies. Mycobacterial killing involved phagosome–lysosome fusion [269] that was induced by the rise of Ca2+ and the activation of PLD resulting from P2X7 activation [270]. It was decreased in macrophages from P2X7 −/− mice [271]. Infection by mycobacteria upregulated the expression of P2X7 and its activation by ATP not only enhanced intracellular bacterial killing but also induced the apoptosis of macrophages [272] or autophagy [273]. This dual response was missing in macrophages from P2X7 −/− mice [271]. ATP-induced bacterial killing was abrogated in macrophages from individuals homozygous for a loss of function P2X7 polymorphism [274] and reduced by 50 % in heterozygous subjects [275]. Additional polymorphisms leading to similar consequences were described later [276]. Furthermore, the pattern of gene expression in response to ATP was different in patients with tuberculosis and controls, suggesting that a defective function of P2X7 might lead to the development of tuberculosis [277]. Infection by parasites, such as Leishmania amazonensis [278, 279] and Toxoplasma gondii [280, 281], also increased the expression of P2X7 that mediated a dual response of parasite killing and macrophage apoptosis.
The P2X7 receptor is also involved in various additional responses of macrophages. ATP released by LPS increased NOS expression and NO production in RAW 264.7 macrophages via P2X7 receptors [282–288]. The P2X7 receptor was also associated with the generation of reactive oxygen species (ROS) [289–291] and leukotriene B4 [279, 292]. Activation of P2X7 receptors on macrophages induces the activation and release of tissue factor and thus favours thrombosis [293, 294]. Phagocytosis of nonopsonised beads and heat-killed bacteria was increased by P2X7 over-expression, showing that it can behave as a scavenger receptor, but this effect was inhibited by ATP [219, 295]. Loss of function polymorphisms of P2X7 and P2X4 receptors were associated with reduced phagocytosis and were overrepresented in patients with macular degeneration [296]. P2X7 receptors play a role in the generation of macrophage-derived giant cells, a hallmark of chronic inflammation [297]. Spontaneous cell fusion was indeed described in macrophage cultures expressing high levels of the P2X7 receptors [298]. Furthermore, the formation of multinucleated giant cells was inhibited by P2X7 antagonists and in macrophages from P2X7-deficient mice [299, 300].
Despite the dominant role of P2X7 in macrophages, evidence has accumulated to support the role of additional receptors. Multiple P2X and P2Y receptor subtypes were identified in mouse J774, spleen and peritoneal macrophages [301]. In an extensive study, mRNA for P2X1, P2X4, P2X5, P2X7, P2Y2, P2Y4, P2Y6, P2Y11, P2Y13 and P2Y14 receptors were all expressed by human alveolar macrophages [302]. It was suggested that other P2X receptor subtypes, in addition to P2X7 receptors, were involved in the ATP-mediated current in human macrophages [303]. In particular it was shown that a small slowly-desensitising ATP-induced current was abolished in P2X4 −/− mice [304]. This P2X4 response might contribute to the P2X7-induced cell death that was reduced by siRNA against P2X4 [305, 306]. It has been reported that HIV binding to macrophages stimulates the release of ATP and that P2X1 is necessary for the entry of HIV in macrophages [307]. P2Y receptors are also expressed and functional. Low concentrations of ATP were shown to activate PLC and IL-6 transcription [308]. Studies of P2Y2 and P2Y4 receptor knockout mice led to the conclusion that P2Y2 receptors are the dominant P2Y receptor subtype in mouse peritoneal macrophages [309]. Nucleotides, released by apoptotic cells, through pannexin 1 [310], act as ‘find-me’ signals to promote P2Y2-dependent recruitment of phagocytic macrophages (as well as monocytes and dendritic cells (DCs)) and this recruitment is reduced in P2Y2-deficient mice [3]. The chemoattractant effect of C5a on macrophages was amplified by the release of ATP and the autocrine stimulation of P2Y2 and also P2Y12 receptors [311]. P2Y2 receptors also mediate potentiation of prostaglandin E2 release involved in the induction of NOS [312, 313] and stimulate the production of monocyte chemoattractant protein-1 (MCP-1)/chemokine (C-C motif) ligand 2 (CCL2) [314]. Furthermore LPS potentiated nucleotide-induced inflammatory gene expression via upregulation of P2Y2 receptors [315]. P2Y6 receptor expression also increased following macrophage activation [309]. Indeed the amount of IL-6 and macrophage inflammatory protein-2 released in response to LPS was significantly enhanced in the presence of UDP, and this effect was lost in the macrophages of P2Y6 knockout mice [316]. Activation of P2Y6 receptors increased the clearance of Escherichia coli and improved survival to peritonitis through the release of MCP-1 and enhancement of macrophage chemotaxis [317]. The P2Y11 receptor was also reported to be functional in macrophages [318]. These authors observed that ATP released from LPS-activated macrophages by vesicular exocytosis activated the P2Y11 receptor, leading to a M1 polarisation characterized by an increased production of IL-12 [318].
Microglia
P1 receptors
The first evidence of a role of adenosine and its receptors in microglia was derived from the observation of effects of propentophylline, a neuroprotective xanthine derivative that increases the extracellular concentration of adenosine by inhibiting its transport into cells [319]. Propentofylline was shown to inhibit the production of ROS by microglial cells [320, 321], their uptake of amyloid precursor protein [322, 323] and their proliferation and release of TNF-α [324]. Further studies showed that microglia express all subtypes of adenosine receptors. Enhanced activation of microglia associated with worsened demyelination and axonal damage was observed in A1 receptor knockout mice subjected to experimental allergic encephalomyelitis [325]. ATP-triggered migration of microglia was inhibited in A1 −/− as well as CD39−/− mice [326]. The A3 receptor is also involved in microglial process extension and migration [327]. On the other hand, ATP acted as a repellent for LPS-treated microglia and induced process retraction; these actions were associated with the upregulation of A2A receptors [328]. A2A receptor knockout mice also displayed enhanced microglial activation in a model of experimental autoimmune encephalomyelitis (EAE) [329].
P2 receptors
It was initially reported that ATP, but not ADP, induced an inward current in microglia [330], associated with an increase in cytosolic Ca2+ [331]. Further pharmacological studies suggested that these responses were mediated by P2Y receptors [332, 333]. It was later shown that the ATP effect on Ca2+ influx was mimicked by BzATP and inhibited by oxATP, supporting the role of the P2z or P2X7 receptor [334]. This receptor was shown to mediate the secretion of IL-1β induced by ATP or by LPS via the release of ATP [335], and to induce microglia cell death [336] as well as microglia-mediated injury of neurons [337]. The P2X7 receptor was also shown to be involved in microglial activation by amyloid β [338]. After nerve injury, the P2X4 receptor was upregulated in the spinal cord and selectively expressed in microglia [339]. The tactile allodynia induced by nerve injury was suppressed by antisense oligodeoxynucleotides silencing P2X4 receptors. Knockdown of the P2X4 receptor by siRNA inhibited migration of microglia [340].
Following brain injury, microglia extrude processes and migrate toward sites of tissue damage. Polarisation, process extension and chemotaxis did not occur in P2Y12-deficient mice, while baseline motility was normal [341]. Furthermore, in living P2Y12-deficient mice, branch extension toward sites of cortical damage was decreased. Microglial activation leads to the downregulation of P2Y12 receptors and the upregulation of P2Y6 receptors [342, 343]. Activation of P2Y6 receptors by UDP stimulates phagocytosis and the uptake of microspheres. In vivo an upregulation of P2Y6 was observed following administration of kainic that damages neurons, leading to microglia activation. Taken together these findings show that ADP, acting through P2Y12, is a find-me signal for microglia, whereas UDP, acting on P2Y6, behaves as an eat-me signal [344] (Fig. 5).
Independence of P2Y12 receptor-mediated migration and P2Y6 receptor-mediated phagocytosis in microglia. a Release/leakage of adenine nucleotides/nucleosides and uridine nucleotides from injured neurons. When neurons or cells are injured or dead, high concentrations of ATP (∼mM) and UTP at a concentration of less than 10 % are leaked. Compared with ATP/ADP/adenosine, UTP/UDP should be transient and localized signals. b Changes in P2Y12 and P2Y6 receptors in microglia according to their activation stages. Insert shows pharmacological characterization of P2Y6 receptor. UDP is a selective agonist to the P2Y6 receptor, and thus, it does not stimulate P2Y12, P2X4, A1, or A2A receptors. Similarly, the P2Y6 receptor is a very selective receptor for UDP, and therefore, is not activated by ATP, ADP, or adenosine (Ado). Resting microglia express no or only faint P2Y6 receptors; whereas, they express P2Y12 receptors adequately. When microglia are activated, they increase P2Y6 receptors; whereas, they decrease P2Y12 receptors. Only when activated microglia meet UDP at the injured sites do they sense UDP as an eat-me signal. c Microglial migration and phagocytosis are controlled by distinct P2 receptors. When microglia sense ATP/ADP by P2Y12 receptors, they extrude their processes, followed by migration toward the injured sites. These microglial motilities are not affected by UDP/P2Y6 receptors. When activated, microglia upregulate P2Y6 receptors, and if they sense the eat-me signal UDP, they start to phagocytose the dead cells or debris. The phagocytic responses are not affected by the activation of P2Y12 receptors nor by other P2 or P1 receptors. (Reproduced from [344], with permission from Springer)
Section summary
ATP released from apoptotic cells constitutes a find-me signal that attracts monocytes/macrophages, an action mediated by the P2Y2 receptor. It stimulates bacterial killing and macrophage apoptosis thereby contributing to decrease the bacterial and parasite burden: this action is mediated by the P2X7 receptor. ATP also exerts a proinflammatory effect through the secretion of IL1-β, which is mediated by the P2X7 receptor and NLRP3 inflammasome.
In contrast, adenosine exerts an inhibitory effect on monocytes/macrophages mediated by A2A and A2B receptors.
Multiple P1 and P2 receptors have been shown to play a role in microglia. The P2X7 receptor is involved in IL-1β secretion and cell death. P2Y12, P2X4, A1 and A3 receptors stimulate process extension and migration, whereas the A2A receptor is inhibitory. On the other hand the P2Y6 receptor is upregulated in activated microglia and triggers microglial phagocytosis.
Dendritic cells
P1 receptors
CD39 and CD73 ectonucleotidases [345] as well as A1, A2A and A3 but not A2B receptors [346] are expressed by human monocyte-derived DCs. In immature DCs, adenosine induced calcium transients but no increase in cAMP. This resulted in actin polymerization, chemotaxis [346] and increased expression of co-stimulatory molecules [347]. Maturation of DCs by LPS resulted in downregulation of A1 and A3 receptor mRNA, whereas A2A receptors were still expressed [346]. In these mature DCs, adenosine increased cAMP and inhibited IL-12 and TNF-α production, whereas it enhanced IL-10 secretion [346, 347]. These results show that adenosine can act as a chemotaxin for immature human DCs and induce their semi-maturation, characterized by a reduced capacity to induce a Th1 polarisation of CD4+ T lymphocytes [347]. Adenosine via cAMP also decreased the capacity of human DCs to prime CD8+ T cells [348].
In murine monocyte-derived DCs, adenosine also impaired maturation and inhibited the production of IL-12, leading to tolerance: this effect was mediated by the A2B receptor instead of the A2A receptor active in human cells [349–351]. IL-27 is a cytokine produced by DCs that suppresses Th1 and Th17 responses and limits inflammation in several experimental models. The suppressive action of IL-27 was mediated at least in part by the induction of CD39 in DCs and the resulting accumulation of adenosine [352]. However, the observation that adenosine could also promote the development of murine Th17 cells, via the A2B receptor- mediated production of IL-6, added an additional complexity [353]. The A2B receptor was upregulated in EAE and A2B knockout mice developed less severe EAE than wild-type mice [354]. In human plasmacytoid DCs, adenosine plays a dual role by initially recruiting immature cells to sites of inflammation, an effect mediated by A1 receptors, and by subsequently inhibiting the production of IL-6 and IFN-α, via the A2A receptor [355].
The physiological importance of the inhibitory effect of adenosine on DCs is supported by observations on the role of ADA. Indeed the high ADA activity of DCs might help to maintain them in an active state [356]. ADA has been shown to be upregulated in DCs from non-obese diabetic (NOD) mice leading to their spontaneous activation and autoimmune T cell activation [357]. Paradoxically DCs from CD39−/− mice exhibited impaired antigen-presenting capacity and ability to induce a Th2 response [358, 359]. This resulted in decreased allergic contact hypersensitivity [358] and allergic airway inflammation [359]. This was explained not by a defect in adenosine formation but by an increased accumulation of ATP leading to the desensitization of P2Y receptors (see below).
Finally it must be mentioned that inosine has been reported to induce DCs chemotaxis independently from adenosine receptors [360]. On the other hand AMP was shown to mimic the inhibitory effects of adenosine on DCs, and these effects were maintained in CD73-deficient mice and could not be explained by adenosine contamination of AMP [361]. The mechanisms of these effects remain unknown.
P2 receptors
Human DCs express mRNA for almost all known P2 receptors [345, 362–364] and extracellular nucleotides exert multiple effects on them ranging from chemotaxis to control of cytokine release and induction of cell death. P2Y but not P2X agonists are potent chemotactic stimuli for immature but not mature DCs [364]. Chemotaxis was associated with a rise in intracellular Ca2+ and actin polymerization and involved the activation of Gi. Allergen challenge was shown to cause acute accumulation of ATP in the airways of asthmatic subjects and mice with experimentally induced asthma that resulted in the recruitment of DCs [1]. That recruitment was mediated by the P2Y2 receptor. Indeed, in vitro the ATP-induced migration of P2Y2-deficient DCs was strongly decreased as compared to DCs from wild-type mice [115]. The attraction of DCs to the lungs in a model of allergic inflammation induced by ovalbumin was also decreased in P2Y2 −/− mice [115]. Decreased attraction of DCs to the airways might also explain the higher mortality of P2Y2 −/− mice with lung infection by pneumonia virus of mice, as a consequence of lowered immune response and viral clearance [365]. Interestingly, the formation of ATP gradients at a site of inflammation can also inhibit transiently the migration of human DCs, via the P2Y11 receptor, and thereby prolong the time of encounter with antigens [366]. Conversely, antagonism of the P2Y11 receptor might improve the migration of antigen-loaded DCs to the lymph nodes. In addition to these direct effects on migration, ATP modulated the expression of chemokine receptors, with an induction of CXCR4 and a reduction of CCR5 [367], and inhibited the release of CCL2 and CCL3 chemokines [368].
Nucleotides were also shown to modulate the maturation of DCs. Schnurr et al. [369] initially reported that ATP stimulates the expression of CD83 and the secretion of IL-12 by human monocyte-derived DCs. This action was shown to be mediated by the P2Y11 receptor and a rise in cAMP [370]. However, la Sala et al. [371] confirmed that ATP stimulates the maturation of DCs but observed an inhibitory effect on the release of IL-12 stimulated by LPS, leading to an impaired ability to initiate Th1 responses. These apparent discrepancies were resolved by the demonstration that ATP, via P2Y11, increased IL-12p40 but inhibited the production of IL-12p70 [372]. Furthermore ATP synergized with LPS and sCD40L to stimulate IL-10 production. This led to the conclusion that ATP, via the P2Y11 receptor, induces a semi-maturation of DCs, characterized by an increased expression of co-stimulatory molecules and a decreased production of bioactive IL-12, leading to increased Th2 responses or tolerance. Additional studies showed that ATP via the P2Y11 receptor produced an impressive upregulation of the expression of thrombospondin-1 and indoleamine 2,3-dioxygenase that could play a major role in tolerance [373]. A systematic study of the effect of ATP on gene expression in DCs revealed a P2Y11-mediated stimulatory effect on the expression of VEGF-A, that has immunosuppressive effects in addition to its angiogenic action [374], and amphiregulin, that can exert an angiogenic and tumorigenic action [375].
Other P2Y receptors were found to be expressed on monocyte-derived DCs. ATP can modulate the function of DCs directly via a cAMP increase mediated by P2Y11 receptors and indirectly via its degradation into ADP, which acts on P2Y1 receptors; these distinct mechanisms combine to inhibit inflammatory cytokine production, particularly IL-12, but have a differential effect on IL-10 [376]. P2Y12 receptors are also expressed by murine DCs and their activation increased antigen endocytosis with subsequent enhancement of T cell activation [377]. UDP, but not UTP, stimulated the release of CXC-chemokine 8 from mature human DCs, via P2Y6 receptors [378]. UTP and UDP also acted on murine DCs to mobilize intracellular Ca2+ and to induce cytokine production [379]. Human immature monocyte-derived DCs express P2Y14 receptors that mediate an increase in [Ca2+]i in response to agonists [380]. In plasmacytoid DCs, UTP, UDP and UDP-glucose were shown to inhibit IFN-α production [381].
Like in macrophages, ATP induced in DCs the NLRP3/ASC inflammasome signalling complexes that drive proteolytic maturation and secretion of the proinflammatory cytokines IL-1β and IL-18 [382, 383]. This action was mediated by the P2X7 receptor, which is functionally expressed on DCs [384]. P2X7 receptors were shown to be present in microvesicles shed from DCs together with IL-1β and caspase-1 and caspase-3 [385]. P2X7-deficient DCs fail to release IL-1β in response to LPS and ATP [386]. This might explain the resistance to allergic contact dermatitis observed in P2X7-deficient mice [386]. Additional P2X7-mediated effects of ATP on DCs include shedding of CD23 [387], release of tissue factor-bearing microparticles [388] and apoptosis [389, 390].
In the intestine ATP released from commensal bacteria induced the differentiation of Th17 CD4+ cells via the activation of lamina propria CD11c+ antigen-presenting cells, apparently via a P2X receptor [391]. The number of Th17 cells was increased in mice deficient in ENTPDase7, which is preferentially expressed on epithelial cells of the small intestine [392].
Section summary
ATP can exert multiple actions on DCs, mediated by distinct receptors: chemotaxis mediated mainly by the P2Y2 receptor; semi-maturation, characterized by increased expression of co-stimulatory molecules and inhibition by IL-12, which is mediated by the P2Y11 receptor and associated with a Th2 response or tolerance; induction of NLRP3/ASC inflammasome signalling complexes, mediated by the P2X7 receptor, that leads to secretion of IL-1β and a proinflammatory effect; and enhanced antigen endocytosis mediated by the P2Y12 receptor.
Adenosine acting on the A2A or A2B receptor exerts complex effects on DCs: as ATP it impairs Th1 polarisation and favours Th2 and/or tolerance, but it can also favour Th17 cell development.
Lymphocytes
T and B lymphocytes
P1 receptors
Adenosine was reported to cause an increase in cAMP in lymphocytes as well as in thymocytes [393–396] and to have powerful inhibitory effects on lymphocyte proliferation [397] and the immune response in humans, particularly those who have inherited deficiency of ADA [398]. The destruction of tumour cells by mouse lymphocytes was shown to be inhibited by adenosine, and this effect was potentiated by an inhibitor of ADA [399]. It was suggested that this effect of adenosine may contribute to the lack of immune response associated with ADA deficiency.
ATPase, ADPase, 5′-nucleotidase and ADA have been shown to be present on human lymphocytes [400–403]. Although it was claimed that adenosine release results from the intracellular degradation of ATP to adenosine, later studies showed that extracellular adenosine is generated following the release of ATP and its extracellular breakdown [404, 405]. Human B lymphocytes showed high degrading activity, while T lymphocytes were reported to be unable to degrade extracellular nucleotides [404]. However, ecto-ATPase activity was reported on cytolytic T lymphocytes [406], and E-NTPDase activity was upregulated within 15 min of T cell stimulation [407]. Furthermore, a subset of T regulatory (Treg) cells expresses CD39 and CD73 ectonucleotidases (see below). However it was suggested that CD39 is not the exclusive switch of the immune system to trigger immunosuppression, and that an alternative adenosine-generating axis is operating [408]. This axis involves the enzymes CD38 (a nicotinamide adenine dinucleotide (NAD+) nucleosidase) and CD303a (an ecto nucleotide pyrophosphatase).
A2A receptors were shown to be expressed on T lymphocytes [409–411]. A2B receptors were also shown to be expressed on human T lymphocytes, and it was suggested that they play a role in lymphocyte deactivation by adenosine [412]. In another study, it was suggested that A2A receptors vary in their expression on T cell functional subsets and may regulate cytokine production in activated T lymphocytes [413]. There was lower expression of A2A receptors on B cells. A3 receptor mRNA and protein were shown to be expressed in both resting and activated human lymphocytes and under activating conditions they are upregulated [414]. Stimulation of A1 and A3 receptors were reported to block the inhibitory action mediated by A2A receptors [415]. Exposure to adenosine prior to antigenic stimulation also induced a desensitization of cAMP accumulation leading to a stronger response to antigenic stimulation [416].
Conclusive evidence for the major role of A2A receptor in the regulation of T lymphocytes came out of the study of A2A-deficient mice. cAMP accumulation in response to adenosine was decreased in T cells from A2A +/− mice and almost abolished in those of A2A −/− mice [417]. In CD4+ T cells, a selective A2A agonist had a major inhibitory effect on the T cell receptor (TCR)-mediated production of IFN-γ and this effect was decreased by 50 % in cells of A2A +/− mice and completely abolished in those from A2A −/− mice [418]. A2A receptor activation inhibited T cell proliferation and IL-2 production whether the cells were expanded under Th1 or Th2-skewing conditions, and again this inhibition was abolished in A2A-deficient mice [419]. Furthermore, TCR stimulation caused a rapid increase in A2A mRNA, both in Th1 and Th2 cells [418, 419].
Adenosine via A2A receptors exerts other effects on T cells. The apoptotic effect of adenosine on resting T cells was inhibited in A2A −/− mice [417, 420]. On the other hand, adenosine via A2A receptor inhibited activation-induced cell death of already activated T cells [421]. Furthermore, the A2A receptor contributes to the maintenance of a normal number of naive T cells by inhibiting TCR-induced activation [422]. Adenosine also inhibits T cell mobility [423], migration to lymph nodes [424] and adhesion to the endothelium [425].
The importance of the A2A-mediated inhibitory effect of adenosine on T cells was underscored by the discovery that CD39 is selectively expressed on Treg cells (see Fig. 6) [426] that are essential for maintaining peripheral tolerance [427, 428]. In human T cells, CD39 is expressed primarily by immunosuppressive Treg cells that express the Foxp3 transcription factor, and its activity is enhanced by TCR ligation [429]. CD73 is also expressed on CD4+/CD25+/Foxp3 Treg cells [430–432]. However, subsets of Treg cells expressing CD39, but not CD73, have been identified [433]. Inhibition of ADA activity further enhanced Treg-mediated immunosuppression [432].
The CD39/CD73 pathway modulates regulatory T cell (Treg) activity. The activation of T cell receptor (TCR), expressed on Tregs, induces CD39 activity. This increment of ATP-metabolizing activity is critical for the immunosuppressive activity of Tregs because it facilitates the pericellular generation of adenosine, a substantial component of the immunosuppressive and anti-inflammatory functions of Tregs. The inhibitory action of Treg-derived adenosine can be ascribed to the activation of A2A receptors expressed on T effector cells, which undergo reduced immune activity. In addition, adenosine generation triggers a self-reinforcing loop of Treg functions because the stimulation of A2A receptors expressed on these cells elicits their expansion and increases their immunoregulatory activity. (Reproduced from [426], with permission from Elsevier)
Several studies have shown the impact of adenosine-mediated inhibition of T cells in various models of disease. Defective adenosine-induced cAMP accumulation and immunosuppression were reported in T lymphocytes of patients with systemic lupus erythematosus [434, 435]. A2A receptor activation during reperfusion after ischemia protected the myocardium from infarction and this effect was dependent on an inhibition of T cell accumulation [436, 437]. A2A receptor agonists attenuated allograft rejection and alloantigen recognition by an action on T lymphocytes [438], suppressed the development of graft-versus-host disease [439, 440] and attenuated experimental autoimmune myasthenia gravis [441]. CD39 and CD73 expressed on Treg cells led to a local accumulation of adenosine that protected against Helicobacter induced gastritis [442]. Treg cells suppressed contact hypersensitivity reactions by a CD39 and adenosine-dependent mechanism [425]. In other models, the action of adenosine proved to be deleterious. A2A-deficient mice were protected from the lethal effect of sepsis, due to preserved lymphocyte function and decreased immunosuppressive IL-10 [443]. CD39 and CD73 expressed on ovarian cancer cells generate adenosine that exerts an immunosuppressive effect, which was relieved by siRNAs against CD39 and CD73 and by an A2A antagonist [444]. In HIV infection, Treg inhibitory effects were relieved by CD39 downregulation and reproduced by an A2A agonist [445, 446]. Furthermore, a polymorphism of the CD39 gene was identified, that is associated with downregulation of CD39 and slower progression to AIDS [446].
Few studies have been performed on B lymphocytes. Accumulation of cAMP produced by adenosine in B cells stimulated by Staphyloccocus aureus suppressed IgM production [447]. On the other hand B cells coexpress CD39 and CD73 and adenosine inhibited B cell proliferation and cytokine expression [448]. Activated B cells also inhibited T cell proliferation and cytokine production [448].
P2 receptors
Early reports showed that ATP protected rat lymphocytes against the loss of intracellular enzymes into the medium [449, 450] and that receptors for ATP were present on lymphocytes [451]. The action of ATP on lymphocytes is complex: ATP was reported to stimulate DNA synthesis in a subpopulations of T cells [452, 453], but ATP was also shown to be highly toxic to human lymphocytes and to thymocytes, causing permeabilization of the plasma membrane and cell death [454, 455]. It was later shown that ATP increased cytosolic Ca2+ in mouse thymocytes [456–458] and stimulated the PLC pathway in human B lymphocytes [459]. On the other hand, an ATP4− receptor-operated sodium channel was identified on human lymphocytes [460, 461]. ATP-gated channels were also identified in human lymphoblasts [462].
Important advances were made in 1994 and the following years with the identification on human lymphocytes of P2Z, now called P2X7, receptors antagonised by oxATP [463] and by the isoquinoline derivative KN-62 [464]. P2X7 receptors were also identified specifically in human B lymphocytes [465, 466] and murine T lymphocytes [467]. P2X7 receptors were implicated in the mitogenic stimulation of human T lymphocytes purified from peripheral blood [468]. ATP and the selective P2X7 agonist BzATP caused plasma membrane depolarisation and a Ca2+ influx in T lymphocytes. ATP or BzATP alone had no effect on lymphocyte proliferation but potentiated the action of mitogens such as anti-CD3 [468]. Transfection of lymphoid cells lacking P2X7 receptors with P2X7 cDNA increased their proliferation [469]. Later studies showed that TCR stimulation triggers the release of ATP through pannexin-1 hemichannels [470] and vesicular exocytosis [471], and upregulates P2X7 expression [472]. siRNA silencing of P2X7 inhibited T cell activation, which was also lower in C57BL/6 mice that express a poorly functional P2X7 receptor, as compared to BALB/c mice that express fully functional P2X7 receptors [472]. Shockwaves increased T cell proliferation through ATP release and P2X7 activation [473]. Thus ATP released through pannexin 1 channels enhances T call activation in an autocrine manner (Fig. 7; [474]). But it is also involved in a paracrine communication that leads to calcium waves in neighbouring lymphocytes and a reduction of T cell motility in lymph nodes that would favour T cell scanning of antigen-loaded DCs [475]. However, P2X7 receptors also induced the shedding of L-selectin (CD62L) from T cells, which accompanies T cell activation and allows T cells to move away from lymph nodes and enter the circulation [476–482].
Purinergic signalling in T cell activation. Antigen recognition by T cells involves the formation of an immune synapse between a T cell and an antigen-presenting cell (APC). The immune synapse contains a large number of signalling molecules that are required for T cell activation, including T cell receptors (TCRs), MHC molecules, co-stimulatory receptors and the purinergic signalling receptors P2X1, P2X4 and P2X7. In response to TCR and CD28 stimulation, pannexin 1, P2X1 receptors and P2X4 receptors translocate to the immune synapse. ATP released through pannexin 1 promotes autocrine signalling via the P2X receptors. Confinement of ATP in the immune synapse results in a powerful autocrine feedback mechanism that facilitates the signal amplification required for antigen recognition. P2 receptors expressed and ATP released by APCs may also have important roles in regulating the antigen recognition process. NFAT nuclear factor of activated T cells. (Reproduced from [474], with permission from Springer)
ATP induced the lysis of CD4+ thymocytes and peripheral CD4+ T cells [483] and the apoptosis of murine thymocytes [484, 485]. T lymphocyte subsets express different levels of P2X7 and high levels are associated with ATP-induced cell death [486]. P2X7 receptor-mediated cell death was also shown to differ between different stages of murine T cell maturation [487]. Interestingly mouse Treg cells express a higher level of P2X7 and their activation by ATP leads to their depletion [488, 489]. P2X7 −/− mice have increased levels of Treg cells [490]. The P2X7 receptor was also involved in T cell death induced by NAD+ through the ADP-ribosylating ectoenzyme, ART2. Indeed ART2-catalyzed ADP-ribosylation activates P2X7 receptors [491–493]. In particular Treg cells express ART2 and can be depleted by intravenous injection of NAD+ [494]. However, ATP (1 mM) enhanced the proliferation and immunosuppressive ability of human Treg cells, whereas it induced apoptosis of CD4+ T cells [495]. The dual action of the P2X7 receptor on growth versus death clearly depends on the concentration of ATP, with stimulatory effects at 250 nM and inhibition at 1 mM [495]. This could be related to the existence of two states of activation of the P2X7 receptor: cation-selective channel or large conductance non-selective pore [496].
Numerous studies have shown the importance of the lymphocyte P2X7 receptor in various models of inflammatory diseases. In some of these models, inhibition or deficiency of P2X7 was associated with decreased immune reactions. Mycobacterium tuberculosis infected P2X7 −/− mice had an increased microbial burden in the lung and pulmonary infiltrates contained a higher number of Treg cells [497]. oxATP was shown to inhibit T cell-mediated autoimmunity in models of autoimmune type 1 diabetes and encephalitis in mice [498]. CD38 knockout NOD mice develop accelerated type 1 diabetes. This was corrected by coablation of P2X7 [499]. oxATP delayed islet allograft rejection [500] and increased cardiac transplant survival in mice [501]; these effects were associated with decreased T cell activation. However in other models P2X7 deficiency was associated with increased immune reactions, illustrating the dual role of P2X7 receptors emphasized previously. Following oral infection with Listeria monocytogenes, P2X7-deficient mice showed enhanced CD8 responses in the intestinal mucosa, which can be explained by the proapoptotic effect of P2X7 on intestinal CD8 cells [502]. Graft versus host disease was enhanced in P2X7 −/− mice, and this is associated with T cell expansion and reduced Treg cells [503]. EAE was also exacerbated in P2X7 −/− mice as a result of decreased apoptosis of T lymphocytes [504] and increased T cell cytokine production [505].
P2X receptors other than P2X7 have been shown to play a role in T cell control. RT-PCR studies had shown that P2X1, P2X2 and P2X6 were expressed by murine thymocytes in addition to P2X7 [506]. ATP released through pannexin hemichannels following TCR stimulation amplified T cell activation not only through P2X7 receptors [472] but also via P2X1 and P2X4 receptors, as demonstrated by the use of siRNA [474, 507]. Hypertonic saline is known to increase T cell function [508]: it acts through the release of ATP and the activation of P2X1, P2X4 and P2X7 receptors, as shown also by gene silencing [509]. Both P2X7 and P2X4 are also involved in the activation of unconventional βγ T cells [510, 511].
Although P2X receptors and particularly P2X7 play a major role in lymphocytes, there is some evidence for the role of P2Y receptors as well. Upregulation of P2Y2 receptor mRNA expression was described as an immediate early gene response in activated thymocytes [512] and P2Y2 receptors were shown to be involved in ATP-induced T cell migration [495]. The P2Y6 receptor was shown to be expressed in activated T cells infiltrating in inflammatory bowel disease [513]. Antagonists of the P2Y6 receptor blocked murine T cell activation [514], but these results must be interpreted with caution since T cells of P2Y6-deficient mice exhibited an increased activity in a model of allergic pulmonary inflammation, suggesting that the P2Y6 receptor plays an inhibitory rather than a stimulatory role [515]. P2Y14 receptors were shown to be functionally expressed by mouse spleen-derived T lymphocytes [516]. Adenine nucleotides inhibited CD4+ T cell activation via an increase in cAMP induced by an unidentified P2Y receptor [517].
Natural killer (NK and NKT) cells
P1 receptors
NK cell activity was shown to be inhibited by adenosine and A2 receptor agonists that increase cAMP [518]. Later studies demonstrated the involvement of A2A receptors [519]. Adenosine via the A2A receptor inhibited IFN-γ production by NKT cells, a subset of T cells with natural killer activity [520], but increased their production of IL-4 and IL-10 [521]. Mice were protected against liver reperfusion injury and concanavalin A (ConA)-induced hepatitis by adenosine acting on the A2A receptor on NKT cells, and this protection was abolished in A2A −/− mice [520, 522]. Sickle cell disease results in disseminated microvascular ischemia and reperfusion injury that leads to the activation of NKT cells and the upregulation of A2A receptors [523–525]. Activation of A2A receptors in NY1DD mice with sickle cell disease reduced pulmonary inflammation and injury [523]. In a phase I study, the A2A agonist regadenoson was administered to patients with sickle cell disease and was shown to inhibit the activation of NKT cells [524]. A2A −/− mice were protected against tumor metastasis, and this protection was associated with increased NK cell maturation and cytotoxic function [526]. On the other hand, an A3 receptor agonist was shown to potentiate NK cell cytotoxic activity [527] and IFN-γ production [528].
P2 receptors
Inhibition of human and mouse NK cell reactivity via nucleotide receptors was reported [529–532]. It was later shown that ATP inhibits cell killing by NK cells via the P2Y11 receptor and an increase in cAMP [533]. On the other hand, NKT cells express the P2X7 receptor, the activation of which can lead to either apoptosis or cell activation [534–536]. In vitro NAD induced rapid apoptosis of NKT cells that was mediated by the P2X7 receptor, but its injection in Con A-treated mice enhanced cytokine production by NK cells and liver injury, that was decreased in P2X7 knockout mice [534]. In CD39-deficient mice, apoptosis of NKT cells was increased leading to protection against ConA-induced liver injury [535] or hyperoxic lung injury [536].
Section summary
The release of ATP through pannexin hemichannels or vesicular exocytosis amplifies in an autocrine way the TCR-mediated activation of T lymphocytes. This amplification is mediated by the P2X7 receptor, and also by P2X1 and P2X4 receptors. But activation of P2X7 can also induce T cell death. The resulting effect (activation or death) depends on the particular subset of T cells and on the concentration of ATP.
Adenosine exerts inhibitory effects on T lymphocytes, which are mediated by the A2A receptor. Treg cells over-express the ectonucleotidases CD39 and CD73 that sequentially convert ATP into AMP and adenosine, and their immunosuppressive action is partially mediated by adenosine.
Concluding remarks
Extracellular nucleotides and adenosine exert a variety of effects on distinct subsets of immune cells via a wide spectrum of receptor subtypes (Table 2). These actions can be both stimulatory and inhibitory, and the balance between the two critically depends on the amount and time course of nucleotide release. This is consistent with the role of ATP and its degradation product adenosine as danger signals that stimulate the immune response following injury but moderate this response when it becomes excessive and deleterious.
Neutrophils and eosinophils
ATP released from neutrophils amplifies their attraction by chemotactic signals via the P2Y2 receptor and after its degradation to adenosine via the A3 receptor, one example of cooperation between P1 and P2 receptors. The P2Y2 receptor is also involved in the recruitment of eosinophils in the lung during allergic inflammation. On the other hand ATP and adenosine have opposite effects on O2 − production and other functions of neutrophils: potentiation by ATP and inhibition by adenosine.
Monocytes/macrophages and microglia
ATP released from apoptotic cells constitutes a find-me signal that attracts monocytes and macrophages, an action mediated by the P2Y2 receptor. Via the P2X7 receptor, ATP stimulates NLRP3 inflammasome activation and IL-1β secretion by macrophages, their killing of bacteria and their apoptosis.
ADP acting on the P2Y12 receptor induces the polarisation and migration of microglia. UDP acting on the P2Y6 receptor stimulates their phagocytic activity. ADP and UDP have, thus, a complementary action of find-me and eat-me signals, respectively, involving a cooperation between two distinct P2Y receptor subtypes. The P2X4, A1 and A3 receptors have also been shown to play a role in microglia migration, whereas the A2A receptor is inhibitory.
Dendritic cells
ATP can exert an immunostimulatory effect on DCs via P2X7 receptor activation. But it can also activate the P2Y11 receptor leading to a semi-maturation state characterized by the upregulation of co-stimulatory molecules and the inhibition of IL-12 production, which impairs the Th1 response and favours tolerance or a Th2 response. The balance between these opposite effects depends on the amount of ATP released and the time course of this release.
Other specific functions of DCs can be activated by nucleotides via distinct P2Y receptor subtypes: chemotaxis by the P2Y2 receptor and antigen endocytosis by the P2Y12 receptor. Adenosine acting on the A2A (human) or A2B (mouse) receptors exerts complex effects on DCs: as ATP it impairs Th1 polarisation and favours Th2 and/or tolerance, but it also favours Th17 cell development.
Lymphocytes
The release of ATP through pannexin hemichannels or vesicular exocytosis amplifies in an autocrine way the TCR-mediated activation of T lymphocytes. This amplification is mediated by the P2X1, P2X4 and P2X7 receptors. On the other hand, Treg cells over-express the ectonucleotidases CD39 and CD73 that sequentially convert ATP into AMP and adenosine, which binds to A2A receptors on effector T cells and suppresses their function.
Neuroimmunology
Contrary to earlier beliefs, the evidence that immune cells are innervated, albeit by nerve varicosities that form occasional close appositions, is convincing. This will be important for future studies of neuroimmunology that might reveal additional roles of ATP and purinergic signalling.
References
Idzko M, Hammad H, van Nimwegen M, Kool M, Willart MA, Muskens F, Hoogsteden HC, Luttmann W, Ferrari D, Di Virgilio F, Virchow JC Jr, Lambrecht BN (2007) Extracellular ATP triggers and maintains asthmatic airway inflammation by activating dendritic cells. Nat Med 13:913–919
Di Virgilio F, Boeynaems JM, Robson SC (2009) Extracellular nucleotides as negative modulators of immunity. Curr Opin Pharmacol 9:507–513
Elliott MR, Chekeni FB, Trampont PC, Lazarowski ER, Kadl A, Walk SF, Park D, Woodson RI, Ostankovich M, Sharma P, Lysiak JJ, Harden TK, Leitinger N, Ravichandran KS (2009) Nucleotides released by apoptotic cells act as a find-me signal to promote phagocytic clearance. Nature 461:282–286
Homolya L, Steinberg TH, Boucher RC (2000) Cell to cell communication in response to mechanical stress via bilateral release of ATP and UTP in polarized epithelia. J Cell Biol 150:1349–1360
McNamara N, Khong A, McKemy D, Caterina M, Boyer J, Julius D, Basbaum C (2001) ATP transduces signals from ASGM1, a glycolipid that functions as a bacterial receptor. Proc Natl Acad Sci U S A 98:9086–9091
Seror C, Melki MT, Subra F, Raza SQ, Bras M, Saidi H, Nardacci R, Voisin L, Paoletti A, Law F, Martins I, Amendola A, Abdul-Sater AA, Ciccosanti F, Delelis O, Niedergang F, Thierry S, Said-Sadier N, Lamaze C, Metivier D, Estaquier J, Fimia GM, Falasca L, Casetti R, Modjtahedi N, Kanellopoulos J, Mouscadet JF, Ojcius DM, Piacentini M, Gougeon ML, Kroemer G, Perfettini JL (2011) Extracellular ATP acts on P2Y2 purinergic receptors to facilitate HIV-1 infection. J Exp Med 208:1823–1834
Lazarowski ER, Shea DA, Boucher RC, Harden TK (2003) Release of cellular UDP-glucose as a potential extracellular signaling molecule. Mol Pharmacol 63:1190–1197
Zhong X, Malhotra R, Guidotti G (2003) ATP uptake in the Golgi and extracellular release require Mcd4 protein and the vacuolar H+-ATPase. J Biol Chem 278:33436–33444
Chekeni FB, Elliott MR, Sandilos JK, Walk SF, Kinchen JM, Lazarowski ER, Armstrong AJ, Penuela S, Laird DW, Salvesen GS, Isakson BE, Bayliss DA, Ravichandran KS (2010) Pannexin 1 channels mediate 'find-me' signal release and membrane permeability during apoptosis. Nature 467:863–867
Forsyth AM, Wan J, Owrutsky PD, Abkarian M, Stone HA (2011) Multiscale approach to link red blood cell dynamics, shear viscosity, and ATP release. Proc Natl Acad Sci U S A 108:10986–10991
Kim JE, Kang TC (2011) The P2X7 receptor-pannexin-1 complex decreases muscarinic acetylcholine receptor-mediated seizure susceptibility in mice. J Clin Invest 121:2037–2047
Anselmi F, Hernandez VH, Crispino G, Seydel A, Ortolano S, Roper SD, Kessaris N, Richardson W, Rickheit G, Filippov MA, Monyer H, Mammano F (2008) ATP release through connexin hemichannels and gap junction transfer of second messengers propagate Ca2+ signals across the inner ear. Proc Natl Acad Sci U S A 105:18770–18775
Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES (2000) The sympathetic nerve - an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev 52:595–638
Serafeim A, Gordon J (2001) The immune system gets nervous. Curr Opin Pharmacol 1:398–403
Bienenstock J, Goetzl EJ, Blennerhassett MG (2003) Autonomic Neuroimmunology. Taylor & Francis, London, pp 139–170
Deaglio S, Robson SC (2011) Ectonucleotidases as regulators of purinergic signaling in thrombosis, inflammation, and immunity. Adv Pharmacol 61:301–332
Burnstock G (1978) A basis for distinguishing two types of purinergic receptor. In: Straub RW, Bolis L (eds) Cell membrane receptors for drugs and hormones: a multidisciplinary approach. Raven Press, New York, pp 107–118
Burnstock G, Kennedy C (1985) Is there a basis for distinguishing two types of P2-purinoceptor? Gen Pharmacol 16:433–440
DePierre JW, Karnovsky ML (1974) Ecto-enzymes of the guinea pig polymorphonuclear leukocyte. I. Evidence for an ecto-adenosine monophosphatase, adenosine triphosphatase, and -p-nitrophenyl phosphates. J Biol Chem 249:7111–7120
Newby AC (1980) Role of adenosine deaminase, ecto-(5'-nucleotidase) and ecto-(non-specific phosphatase) in cyanide-induced adenosine monophosphate catabolism in rat polymorphonuclear leucocytes. Biochem J 186:907–918
Smith GP, Peters TJ (1981) Subcellular localization and properties of pyridoxal phosphate phosphatases of human polymorphonuclear leukocytes and their relationship to acid and alkaline phosphatase. Biochim Biophys Acta 661:287–294
Eltzschig HK, Weissmuller T, Mager A, Eckle T (2006) Nucleotide metabolism and cell-cell interactions. Methods Mol Biol 341:73–87
Chen Y, Shukla A, Namiki S, Insel PA, Junger WG (2004) A putative osmoreceptor system that controls neutrophil function through the release of ATP, its conversion to adenosine, and activation of A2 adenosine and P2 receptors. J Leukoc Biol 76:245–253
Chen Y, Corriden R, Inoue Y, Yip L, Hashiguchi N, Zinkernagel A, Nizet V, Insel PA, Junger WG (2006) ATP release guides neutrophil chemotaxis via P2Y2 and A3 receptors. Science 314:1792–1795
Cronstein BN, Kramer SB, Weissmann G, Hirschhorn R (1983) Adenosine: a physiological modulator of superoxide anion generation by human neutrophils. J Exp Med 158:1160–1177
Cronstein BN, Rosenstein ED, Kramer SB, Weissmann G, Hirschhorn R (1985) Adenosine; a physiologic modulator of superoxide anion generation by human neutrophils. Adenosine acts via an A2 receptor on human neutrophils. J Immunol 135:1366–1371
Cronstein BN, Kubersky SM, Weissmann G, Hirschhorn R (1987) Engagement of adenosine receptors inhibits hydrogen peroxide (H2O2 −) release by activated human neutrophils. Clin Immunol Immunopathol 42:76–85
Schrier DJ, Imre KM (1986) The effects of adenosine agonists on human neutrophil function. J Immunol 137:3284–3289
Sun WC, Moore JN, Hurley DJ, Vandenplas ML, Murray TF (2007) Effects of stimulation of adenosine A2A receptors on lipopolysaccharide-induced production of reactive oxygen species by equine neutrophils. Am J Vet Res 68:649–656
Colli S, Tremoli E (1991) Multiple effects of dipyridamole on neutrophils and mononuclear leukocytes: adenosine-dependent and adenosine-independent mechanisms. J Lab Clin Med 118:136–145
Mircevová L, Viktora L, Hermanová E (1984) Inhibition of phagocytosis of polymorphonuclear leucocytes by adenosine and HoCl3 in vitro. Med Biol 62:326–330
Hardart GE, Sullivan GW, Carper HT, Mandell GL (1991) Adenosine and 2-phenylaminoadenosine (CV-1808) inhibit human neutrophil bactericidal function. Infect Immun 59:885–889
Laghi Pasini F, Capecchi PL, Ceccatelli L, Orrico A, Pasqui AL, Di Perri T (1986) Effect of extracellular Ca++ on in vitro adenosine-dependent inhibition of neutrophil function. Int J Immunotherapy 11:225–232
Laghi Pasini F, Capecchi PL, Pasqui AL, Ceccatelli L, Mazza S, Gistri A, Di Perri T (1990) Adenosine system and cell calcium translocation: interference of calcium channel blockers. Exp Gerontol 25:383–391
Tsuruta S, Ito S, Mikawa H (1992) Adenosine inhibits divalent cation influx across human neutrophil plasma membrane via surface adenosine A2 receptors. Cell Signal 4:543–551
Nielson CP, Vestal RE (1989) Effects of adenosine on polymorphonuclear leucocyte function, cyclic 3': 5'-adenosine monophosphate, and intracellular calcium. Br J Pharmacol 97:882–888
Zhang Y, Palmblad J, Fredholm BB (1996) Biphasic effect of ATP on neutrophil functions mediated by P2U and adenosine A2A receptors. Biochem Pharmacol 51:957–965
Thibault N, Burelout C, Harbour D, Borgeat P, Naccache PH, Bourgoin SG (2002) Occupancy of adenosine A2a receptors promotes fMLP-induced cyclic AMP accumulation in human neutrophils: impact on phospholipase D activity and recruitment of small GTPases to membranes. J Leukoc Biol 71:367–377
Varani K, Portaluppi F, Gessi S, Merighi S, Vincenzi F, Cattabriga E, Dalpiaz A, Bortolotti F, Belardinelli L, Borea PA (2005) Caffeine intake induces an alteration in human neutrophil A2A adenosine receptors. Cell Mol Life Sci 62:2350–2358
McColl SR, St-Onge M, Dussault AA, Laflamme C, Bouchard L, Boulanger J, Pouliot M (2006) Immunomodulatory impact of the A2A adenosine receptor on the profile of chemokines produced by neutrophils. FASEB J 20:187–189
Grenz A, Kim JH, Bauerle JD, Tak E, Eltzschig HK, Clambey ET (2012) Adora2b adenosine receptor signaling protects during acute kidney injury via inhibition of neutrophil-dependent TNF-α release. J Immunol 189:4566–4573
van der Hoeven D, Wan TC, Gizewski ET, Kreckler LM, Maas JE, Van Orman J, Ravid K, Auchampach JA (2011) A role for the low-affinity A2B adenosine receptor in regulating superoxide generation by murine neutrophils. J Pharmacol Exp Ther 338:1004–1012
van der Hoeven D, Wan TC, Auchampach JA (2008) Activation of the A3 adenosine receptor suppresses superoxide production and chemotaxis of mouse bone marrow neutrophils. Mol Pharmacol 74:685–696
Bouma MG, Jeunhomme TM, Boyle DL, Dentener MA, Voitenok NN, van den Wildenberg FA, Buurman WA (1997) Adenosine inhibits neutrophil degranulation in activated human whole blood: involvement of adenosine A2 and A3 receptors. J Immunol 158:5400–5408
Krump E, Picard S, Mancini J, Borgeat P (1997) Suppression of leukotriene B4 biosynthesis by endogenous adenosine in ligand-activated human neutrophils. J Exp Med 186:1401–1406
Cadieux JS, Leclerc P, St-Onge M, Dussault AA, Laflamme C, Picard S, Ledent C, Borgeat P, Pouliot M (2005) Potentiation of neutrophil cyclooxygenase-2 by adenosine: an early anti-inflammatory signal. J Cell Sci 118:1437–1447
Garcia-Castro I, Mato JM, Vasanthakumar G, Wiesmann WP, Schiffmann E, Chiang PK (1983) Paradoxical effects of adenosine on neutrophil chemotaxis. J Biol Chem 258:4345–4349
Rose FR, Hirschhorn R, Weissmann G, Cronstein BN (1988) Adenosine promotes neutrophil chemotaxis. J Exp Med 167:1186–1194
Salmon JE, Cronstein BN (1990) Fcγ Receptor-mediated functions in neutrophils are modulated by adenosine receptor occupancy. A1 receptors are stimulatory and A2 receptors are inhibitory. J Immunol 145:2235–2240
Aeffner F, Woods PS, Davis IC (2014) Activation of A 1-adenosine receptors promotes leukocyte recruitment to the lung and attenuates acute lung injury in mice infected with influenza A/WSN/33 (H1N1) virus. J Virol 88:10214–10227
Reutershan J, Cagnina RE, Chang D, Linden J, Ley K (2007) Therapeutic anti-inflammatory effects of myeloid cell adenosine receptor A2a stimulation in lipopolysaccharide-induced lung injury. J Immunol 179:1254–1263
Konrad FM, Witte E, Vollmer I, Stark S, Reutershan J (2012) Adenosine receptor A2b on hematopoietic cells mediates LPS-induced migration of PMNs into the lung interstitium. Am J Physiol Lung Cell Mol Physiol 303:L425–L438
Inoue Y, Chen Y, Hirsh MI, Yip L, Junger WG (2008) A3 and P2Y2 receptors control the recruitment of neutrophils to the lungs in a mouse model of sepsis. Shock 30:173–177
Butler M, Sanmugalingam D, Burton VJ, Wilson T, Pearson R, Watson RP, Smith P, Parkinson SJ (2012) Impairment of adenosine A3 receptor activity disrupts neutrophil migratory capacity and impacts innate immune function in vivo. Eur J Immunol 42:3358–3368
Bao Y, Chen Y, Ledderose C, Li L, Junger WG (2013) Pannexin 1 channels link chemoattractant receptor signalling to local excitation and global inhibition responses at the front and back of polarized neutrophils. J Biol Chem 288:22650–22657
Corriden R, Self T, Akong-Moore K, Nizet V, Kellam B, Briddon SJ, Hill SJ (2013) Adenosine-A3 receptors in neutrophil microdomains promote the formation of bacteria-tethering cytonemes. EMBO Rep 14:726–732
Cronstein BN, Levin RI, Philips M, Hirschhorn R, Abramson SB, Weissmann G (1992) Neutrophil adherence to endothelium is enhanced via adenosine A1 receptors and inhibited via adenosine A2 receptors. J Immunol 148:2201–2206
Asako H, Wolf RE, Granger DN (1993) Leukocyte adherence in rat mesenteric venules: effects of adenosine and methotrexate. Gastroenterology 104:31–37
Eltzschig HK, Thompson LF, Karhausen J, Cotta RJ, Ibla JC, Robson SC, Colgan SP (2004) Endogenous adenosine produced during hypoxia attenuates neutrophil accumulation: coordination by extracellular nucleotide metabolism. Blood 104:3986–3992
Sullivan GW, Lee DD, Ross WG, DiVietro JA, Lappas CM, Lawrence MB, Linden J (2004) Activation of A2A adenosine receptors inhibits expression of α4/β1 integrin (very late antigen-4) on stimulated human neutrophils. J Leukoc Biol 75:127–134
Thiel M, Chambers JD, Chouker A, Fischer S, Zourelidis C, Bardenheuer HJ, Arfors KE, Peter K (1996) Effect of adenosine on the expression of β2 integrins and L-selectin of human polymorphonuclear leukocytes in vitro. J Leukoc Biol 59:671–682
Zhao ZQ, Sato H, Williams MW, Fernandez AZ, Vinten-Johansen J (1996) Adenosine A2-receptor activation inhibits neutrophil-mediated injury to coronary endothelium. Am J Physiol 271:H1456–H1464
Eltzschig HK, MacManus CF, Colgan SP (2008) Neutrophils as sources of extracellular nucleotides: functional consequences at the vascular interface. Trends Cardiovasc Med 18:103–107
Corriden R, Chen Y, Inoue Y, Beldi G, Robson SC, Insel PA, Junger WG (2008) Ecto-nucleoside triphosphate diphosphohydrolase 1 (E-NTPDase1/CD39) regulates neutrophil chemotaxis by hydrolyzing released ATP to adenosine. J Biol Chem 283:28480–28486
Kilian JG, Nakhla S, Sieveking DP, Celermajer DS (2005) Adenosine prevents neutrophil adhesion to human endothelial cells after hypoxia/reoxygenation. Int J Cardiol 105:322–326
Watanabe T, Tokuyama S, Yasuda M, Sasaki T, Yamamoto T (2002) Involvement of adenosine A2 receptors in the changes of tissue factor-dependent coagulant activity induced by polymorphonuclear leukocytes in endothelial cells. Jpn J Pharmacol 88:407–413
Pospísil M, Hofer M, Znojil V, Vácha J, Netiková J, Holá J (1995) Synergistic effect of granulocyte colony-stimulating factor and drugs elevating extracellular adenosine on neutrophil production in mice. Blood 86:3692–3697
Yasui K, Agematsu K, Shinozaki K, Hokibara S, Nagumo H, Nakazawa T, Komiyama A (2000) Theophylline induces neutrophil apoptosis through adenosine A2A receptor antagonism. J Leukoc Biol 67:529–535
Fortin A, Harbour D, Fernandes M, Borgeat P, Bourgoin S (2006) Differential expression of adenosine receptors in human neutrophils: up-regulation by specific Th1 cytokines and lipopolysaccharide. J Leukoc Biol 79:574–585
Bazzichi L, Trincavelli L, Rossi A, De Feo F, Lucacchini A, Bombardieri S, Martini C (2005) A2B adenosine receptor activity is reduced in neutrophils from patients with systemic sclerosis. Arthritis Res Ther 7:R189–R195
Kaufmann I, Hoelzl A, Schliephake F, Hummel T, Chouker A, Lysenko L, Peter K, Thiel M (2007) Effects of adenosine on functions of polymorphonuclear leukocytes from patients with septic shock. Shock 27:25–31
Inoue Y, Chen Y, Pauzenberger R, Hirsh MI, Junger WG (2008) Hypertonic saline up-regulates A3 adenosine receptor expression of activated neutrophils and increases acute lung injury after sepsis. Crit Care Med 36:2569–2575
Varani K, Gessi S, Merighi S, Iannotta V, Cattabriga E, Spisani S, Cadossi R, Borea PA (2002) Effect of low frequency electromagnetic fields on A2A adenosine receptors in human neutrophils. Br J Pharmacol 136:57–66
Varani K, Gessi S, Merighi S, Iannotta V, Cattabriga E, Pancaldi C, Cadossi R, Borea PA (2003) Alteration of A3 adenosine receptors in human neutrophils and low frequency electromagnetic fields. Biochem Pharmacol 66:1897–1906
Kuroki M, Takeshige K, Minakami S (1989) ATP-induced calcium mobilization in human neutrophils. Biochim Biophys Acta 1012:103–106
Saito H, Ebisawa M, Reason DC, Ohno K, Kurihara K, Sakaguchi N, Ohgimi A, Saito E, Akasawa A, Akimoto K (1991) Extracellular ATP stimulates interleukin-dependent cultured mast cells and eosinophils through calcium mobilization. Int Arch Allergy Appl Immunol 94:68–70
Kuhns DB, Wright DG, Nath J, Kaplan SS, Basford RE (1988) ATP induces transient elevations of [Ca2+] i in human neutrophils and primes these cells for enhanced O2 − generation. Lab Invest 58:448–453
Seifert R, Wenzel K, Eckstein F, Schultz G (1989) Purine and pyrimidine nucleotides potentiate activation of NADPH oxidase and degranulation by chemotactic peptides and induce aggregation of human neutrophils via G proteins. Eur J Biochem 181:277–285
Tuluc F, Bredetean O, Brailoiu E, Meshki J, Garcia A, Dun NJ, Kunapuli SP (2005) The priming effect of extracellular UTP on human neutrophils: Role of calcium released from thapsigargin-sensitive intracellular stores. Purinergic Signal 1:359–368
Ward PA, Cunningham TW, McCulloch KK, Phan SH, Powell J, Johnson KJ (1988) Platelet enhancement of O2 − responses in stimulated human neutrophils. Identification of platelet factor as adenine nucleotide. Lab Invest 58:37–47
Ward PA, Cunningham TW, McCulloch KK, Johnson KJ (1988) Regulatory effects of adenosine and adenine nucleotides on oxygen radical responses of neutrophils. Lab Invest 58:438–447
Axtell RA, Sandborg RR, Smolen JE, Ward PA, Boxer LA (1990) Exposure of human neutrophils to exogenous nucleotides causes elevation in intracellular calcium, transmembrane calcium fluxes, and an alteration of a cytosolic factor resulting in enhanced superoxide production in response to FMLP and arachidonic acid. Blood 75:1324–1332
Cockcroft S, Stutchfield J (1989) The receptors for ATP and fMetLeuPhe are independently coupled to phospholipases C and A2 via G-protein(s). Relationship between phospholipase C and A2 activation and exocytosis in HL60 cells and human neutrophils. Biochem J 263:715–723
Cockcroft S, Stutchfield J (1989) ATP stimulates secretion in human neutrophils and HL60 cells via a pertussis toxin-sensitive guanine nucleotide-binding protein coupled to phospholipase C. FEBS Lett 245:25–29
Ford-Hutchinson AW (1982) Aggregation of rat neutrophils by nucleotide triphosphates. Br J Pharmacol 76:367–371
O'Grady SM (2012) Purinergic signaling and immune cell chemotaxis. Focus on "the UDP-sugar-sensing P2Y14 receptor promotes Rho-mediated signaling and chemotaxis in human neutrophils". Am J Physiol Cell Physiol 303:C486–C487
Cicko S, Lucattelli M, Muller T, Lommatzsch M, De Cunto G, Cardini S, Sundas W, Grimm M, Zeiser R, Durk T, Zissel G, Boeynaems JM, Sorichter S, Ferrari D, Di Virgilio F, Virchow JC, Lungarella G, Idzko M (2010) Purinergic receptor inhibition prevents the development of smoke-induced lung injury and emphysema. J Immunol 185:688–697
Ayata CK, Ganal SC, Hockenjos B, Willim K, Vieira RP, Grimm M, Robaye B, Boeynaems JM, Di Virgilio F, Pellegatti P, Diefenbach A, Idzko M, Hasselblatt P (2012) Purinergic P2Y2 receptors promote neutrophil infiltration and hepatocyte death in mice with acute liver injury. Gastroenterology 143:1620–1629
Scrivens M, Dickenson JM (2006) Functional expression of the P2Y14 receptor in human neutrophils. Eur J Pharmacol 543:166–173
Sesma JI, Kreda SM, Steinckwich-Besancon N, Dang H, García-Mata R, Harden TK, Lazarowski ER (2012) The UDP-sugar-sensing P2Y14 receptor promotes Rho-mediated signaling and chemotaxis in human neutrophils. Am J Physiol Cell Physiol 303:C490–C498
Barrett MO, Sesma JI, Ball CB, Jayasekara PS, Jacobson KA, Lazarowski ER, Harden TK (2013) A selective high-affinity antagonist of the P2Y14 receptor inhibits UDP-glucose-stimulated chemotaxis of human neutrophils. Mol Pharmacol 84:41–49
Vaughan KR, Stokes L, Prince LR, Marriott HM, Meis S, Kassack MU, Bingle CD, Sabroe I, Surprenant A, Whyte MK (2007) Inhibition of neutrophil apoptosis by ATP is mediated by the P2Y11 receptor. J Immunol 179:8544–8553
Alkayed F, Kashimata M, Koyama N, Hayashi T, Tamura Y, Azuma Y (2012) P2Y11 purinoceptor mediates the ATP-enhanced chemotactic response of rat neutrophils. J Pharmacol Sci 120:288–295
Suh BC, Kim JS, Namgung U, Ha H, Kim KT (2001) P2X7 nucleotide receptor mediation of membrane pore formation and superoxide generation in human promyelocytes and neutrophils. J Immunol 166:6754–6763
Nagaoka I, Tamura H, Hirata M (2006) An antimicrobial cathelicidin peptide, human CAP18/LL-37, suppresses neutrophil apoptosis via the activation of formyl-peptide receptor-like 1 and P2X7. J Immunol 176:3044–3052
Christenson K, Björkman L, Tängemo C, Bylund J (2008) Serum amyloid A inhibits apoptosis of human neutrophils via a P2X7-sensitive pathway independent of formyl peptide receptor-like 1. J Leukoc Biol 83:139–148
da Silva GL, Sperotto ND, Borges TJ, Bonorino C, Takyia CM, Coutinho-Silva R, Campos MM, Zanin RF, Morrone FB (2013) P2X7 receptor is required for neutrophil accumulation in a mouse model of irritant contact dermatitis. Exp Dermatol 22:184–188
Martel-Gallegos G, Rosales-Saavedra MT, Reyes JP, Casas-Pruneda G, Toro-Castillo C, Pérez-Cornejo P, Arreola J (2010) Human neutrophils do not express purinergic P2X7 receptors. Purinergic Signal 6:297–306
Mohanty JG, Raible DG, McDermott LJ, Pelleg A, Schulman ES (2001) Effects of purine and pyrimidine nucleotides on intracellular Ca 2+ in human eosinophils: activation of purinergic P2Y receptors. J Allergy Clin Immunol 107:849–855
Lecut C, Frederix K, Johnson DM, Deroanne C, Thiry M, Faccinetto C, Marée R, Evans RJ, Volders PG, Bours V, Oury C (2009) P2X1 ion channels promote neutrophil chemotaxis through Rho kinase activation. J Immunol 183:2801–2809
Lecut C, Faccinetto C, Delierneux C, van Oerle R, Spronk HM, Evans RJ, El BJ, Bours V, Oury C (2012) ATP-gated P2X1 ion channels protect against endotoxemia by dampening neutrophil activation. J Thromb Haemost 10:453–465
Kohno Y, Ji X, Mawhorter SD, Koshiba M, Jacobson KA (1996) Activation of A3 adenosine receptors on human eosinophils elevates intracellular calcium. Blood 88:3569–3574
Walker BA (1996) Effects of adenosine on guinea pig pulmonary eosinophils. Inflammation 20:11–21
Ezeamuzie CI, Philips E (1999) Adenosine A3 receptors on human eosinophils mediate inhibition of degranulation and superoxide anion release. Br J Pharmacol 127:188–194
Knight D, Zheng X, Rocchini C, Jacobson M, Bai T, Walker B (1997) Adenosine A3 receptor stimulation inhibits migration of human eosinophils. J Leukoc Biol 62:465–468
Walker BA, Jacobson MA, Knight DA, Salvatore CA, Weir T, Zhou D, Bai TR (1997) Adenosine A3 receptor expression and function in eosinophils. Am J Respir Cell Mol Biol 16:531–537
Young HW, Molina JG, Dimina D, Zhong H, Jacobson M, Chan LN, Chan TS, Lee JJ, Blackburn MR (2004) A3 adenosine receptor signaling contributes to airway inflammation and mucus production in adenosine deaminase-deficient mice. J Immunol 173:1380–1389
Burgers JA, Schweizer RC, Koenderman L, Bruijnzeel PL, Akkerman JW (1993) Human platelets secrete chemotactic activity for eosinophils. Blood 81:49–55
Dichmann S, Idzko M, Zimpfer U, Hofmann C, Ferrari D, Luttmann W, Virchow C Jr, Di Virgilio F, Norgauer J (2000) Adenosine triphosphate-induced oxygen radical production and CD11b up-regulation: Ca++ mobilization and actin reorganization in human eosinophils. Blood 95:973–978
Ferrari D, Idzko M, Dichmann S, Purlis D, Virchow C, Norgauer J, Chiozzi P, Di Virgilio F, Luttmann W (2000) P2 purinergic receptors of human eosinophils: characterization and coupling to oxygen radical production. FEBS Lett 486:217–224
Idzko M, Dichmann S, Panther E, Ferrari D, Herouy Y, Virchow C Jr, Luttmann W, Di Virgilio F, Norgauer J (2001) Functional characterization of P2Y and P2X receptors in human eosinophils. J Cell Physiol 188:329–336
Idzko M, Panther E, Bremer HC, Sorichter S, Luttmann W, Virchow CJ Jr, Di Virgilio F, Herouy Y, Norgauer J, Ferrari D (2003) Stimulation of P2 purinergic receptors induces the release of eosinophil cationic protein and interleukin-8 from human eosinophils. Br J Pharmacol 138:1244–1250
Kobayashi T, Kouzaki H, Kita H (2010) Human eosinophils recognize endogenous danger signal crystalline uric acid and produce proinflammatory cytokines mediated by autocrine ATP. J Immunol 184:6350–6358
Muniz VS, Thompson GA, Barbosa-Pereira C, Patrasso-Salgado B, Neves JS (2011) Expression and functional roles of the purinergic receptor P2Y12 in human eosinophils. Inflamm Res 60:S145–S146
Müller T, Robaye B, Vieira RP, Ferrari D, Grimm M, Jakob T, Martin SF, Di Virgilio F, Boeynaems JM, Virchow JC, Idzko M (2010) The purinergic receptor P2Y2 receptor mediates chemotaxis of dendritic cells and eosinophils in allergic lung inflammation. Allergy 65:1545–1553
Vanderstocken G, Bondue B, Horckmans M, Di PL, Robaye B, Boeynaems JM, Communi D (2010) P2Y2 receptor regulates VCAM-1 membrane and soluble forms and eosinophil accumulation during lung inflammation. J Immunol 185:3702–3707
Marone G, Findlay SR, Lichtenstein LM (1979) Adenosine receptor on human basophils: modulation of histamine release. J Immunol 123:1473–1477
Marone G, Triggiani M, Kagey-Sobotka A, Lichtenstein LM, Condorelli M (1986) Adenosine receptors on human basophils and lung mast cells. Adv Exp Med Biol 195 Pt B:35–42
Church MK, Holgate ST, Hughes PJ (1983) Adenosine inhibits and potentiates IgE-dependent histamine release from human basophils by an A2-receptor mediated mechanism. Br J Pharmacol 80:719–726
Marone G, Vigorita S, Antonelli C, Torella G, Genovese A, Condorelli M (1985) Evidence for an adenosine A2/Ra receptor on human basophils. Life Sci 36:339–345
Hughes PJ, Church MK (1986) Inhibition of immunological and nonimmunological histamine release from human basophils by adenosine analogues that act at P-sites. Biochem Pharmacol 35:1809–1816
Ludowyke RI, Scurr LL (1994) Calcium-independent secretion by ATP gamma S from a permeabilized rat basophilic leukaemia cell line (RBL-2H3). Cell Signal 6:223–231
Nakano M, Kudo F, Nakamura T, Kasai K, Ito K, Takami H, Ito K (2013) Uracil nucleotides enhance the degranulation of human basophils induced by anti-IgE antibody via a purinergic receptor (P6016). J Immunol 190:59
Marquardt DL, Parker CW, Sullivan TJ (1978) Potentiation of mast cell mediator release by adenosine. J Immunol 120:871–878
Burt DS, Stanworth DR (1983) The effect of ribose and purine modified adenosine analogues on the secretion of histamine from rat mast cells induced by ionophore A23187. Biochem Pharmacol 32:2729–2732
Hughes PJ, Holgate ST, Church MK (1984) Adenosine inhibits and potentiates IgE-dependent histamine release from human lung mast cells by an A2-purinoceptor mediated mechanism. Biochem Pharmacol 33:3847–3852
Church MK, Hughes PJ (1985) Adenosine potentiates immunological histamine release from rat mast cells by a novel cyclic AMP-independent cell-surface action. Br J Pharmacol 85:3–5
Church MK, Hughes PJ, Vardey CJ (1986) Studies on the receptor mediating cyclic AMP-independent enhancement by adenosine of IgE-dependent mediator release from rat mast cells. Br J Pharmacol 87:233–242
Leoutsakos A, Pearce FL (1986) The effect of adenosine and its analogues on cyclic AMP changes and histamine secretion from rat peritoneal mast cells stimulated by various ligands. Biochem Pharmacol 35:1373–1379
Campos BG, Ferreira RR, Gomes JC (2000) The potentiation of the histamine release induced by adenosine in mast cells from guinea pig lung and heart: sharp dependence on the time of preincubation. Pharmacol Res 41:291–297
Marquardt DL, Walker LL, Wasserman SI (1984) Adenosine receptors on mouse bone marrow-derived mast cells: functional significance and regulation by aminophylline. J Immunol 133:932–937
Delmich K, Eichelberg D, Schmutzler W (1985) The effects of adenosine and of some adenosine analogues on the concanavalin A- or acetylcholine-induced histamine release from human adenoidal mast cells. Agents Actions 16:141–143
Lohse MJ, Maurer K, Gensheimer HP, Schwabe U (1987) Dual actions of adenosine on rat peritoneal mast cells. Naunyn Schmiedebergs Arch Pharmacol 335:555–560
Auchampach JA, Jin X, Wan TC, Caughey GH, Linden J (1997) Canine mast cell adenosine receptors: cloning and expression of the A3 receptor and evidence that degranulation is mediated by the A2B receptor. Mol Pharmacol 52:846–860
Ramkumar V, Stiles GL, Beaven MA, Ali H (1993) The A3 adenosine receptor is the unique adenosine receptor which facilitates release of allergic mediators in mast cells. J Biol Chem 268:16887–16890
Fozard JR, Pfannkuche HJ, Schuurman HJ (1996) Mast cell degranulation following adenosine A3 receptor activation in rats. Eur J Pharmacol 298:293–297
Zhong H, Shlykov SG, Molina JG, Sanborn BM, Jacobson MA, Tilley SL, Blackburn MR (2003) Activation of murine lung mast cells by the adenosine A3 receptor. J Immunol 171:338–345
Tilley SL, Wagoner VA, Salvatore CA, Jacobson MA, Koller BH (2000) Adenosine and inosine increase cutaneous vasopermeability by activating A3 receptors on mast cells. J Clin Invest 105:361–367
Tilley SL, Tsai M, Williams CM, Wang ZS, Erikson CJ, Galli SJ, Koller BH (2003) Identification of A3 receptor- and mast cell-dependent and -independent components of adenosine-mediated airway responsiveness in mice. J Immunol 171:331–337
Peachell PT, Lichtenstein LM, Schleimer RP (1991) Differential regulation of human basophil and lung mast cell function by adenosine. J Pharmacol Exp Ther 256:717–726
Gomez G, Nardone V, Lotfi-Emran S, Zhao W, Schwartz LB (2013) Intracellular adenosine inhibits IgE-dependent degranulation of human skin mast cells. J Clin Immunol 33:1349–1359
Marquardt DL, Walker LL, Heinemann S (1994) Cloning of two adenosine receptor subtypes from mouse bone marrow-derived mast cells. J Immunol 152:4508–4515
Hua X, Chason KD, Jania C, Acosta T, Ledent C, Tilley SL (2013) Gs-coupled adenosine receptors differentially limit antigen-induced mast cell activation. J Pharmacol Exp Ther 344:426–435
Feoktistov I, Ryzhov S, Goldstein AE, Biaggioni I (2003) Mast cell-mediated stimulation of angiogenesis: cooperative interaction between A2B and A3 adenosine receptors. Circ Res 92:485–492
Ryzhov S, Zaynagetdinov R, Goldstein AE, Novitskiy SV, Dikov MM, Blackburn MR, Biaggioni I, Feoktistov I (2008) Effect of A2B adenosine receptor gene ablation on proinflammatory adenosine signaling in mast cells. J Immunol 180:7212–7220
Hua X, Chason KD, Patel JY, Naselsky WC, Tilley SL (2011) IL-4 amplifies the pro-inflammatory effect of adenosine in human mast cells by changing expression levels of adenosine receptors. PLoS One 6:e24947
Keller R (1966) Tissue mast cells in immune reactions. Monogr Allergy 2:1–144
Diamant B, Krüger PG (1967) Histamine release from isolated rat peritoneal mast cells induced by adenosine-5'-triphosphate. Acta Physiol Scand 71:291–302
Dahlquist R, Diamant B (1970) Further observations on ATP-induced histamine release from rat mast cells. Acta Pharmacol Toxicol (Copenh) 28:43
Sugiyama K (1971) Calcium-dependent histamine release with degranulation from isolated rat mast cells by adenosine 5'-triphosphate. Jpn J Pharmacol 21:209–226
Krüger G, Bloom D, Diamant B (1974) Structural aspects of histamine release in rat peritoneal mast cells. Effects of adenosine 5'-triphosphate and role of calcium. Int Arch Allergy Appl Immunol 47:1–13
Cockcroft S, Gomperts BD (1979) Activation and inhibition of calcium-dependent histamine secretion by ATP ions applied to rat mast cells. J Physiol 296:229–243
Kiernan JA (1972) Effects of known and suspected neurotransmitter substances and of some nucleotides on isolated mast cells. Experientia 28:653–655
Bienenstock J, MacQueen G, Sestini P, Marshall JS, Stead RH, Perdue MH (1991) Mast cell/nerve interactions in vitro and in vivo. Am Rev Respir Dis 143:S55–S58
Grosman N, Diamant B (1975) Effects of adenosine-5'-triphosphate (ATP) on rat mast cells: influence on anaphylactic and compound 48/80-induced histamine release. Agents Actions 5:108–114
Johansen T, Chakravarty N (1975) The utilization of adenosine triphosphate in rat mast cells during histamine release induced by anaphylactic reaction and compound 48/80. Naunyn Schmiedebergs Arch Pharmacol 288:243–260
Bulanova E, Budagian V, Orinska Z, Hein M, Petersen F, Thon L, Adam D, Bulfone-Paus S (2005) Extracellular ATP induces cytokine expression and apoptosis through P2X7 receptor in murine mast cells. J Immunol 174:3880–3890
Tatham PE, Lindau M (1990) ATP-induced pore formation in the plasma membrane of rat peritoneal mast cells. J Gen Physiol 95:459–476
Kurashima Y, Amiya T, Nochi T, Fujisawa K, Haraguchi T, Iba H, Tsutsui H, Sato S, Nakajima S, Iijima H, Kubo M, Kunisawa J, Kiyono H (2012) Extracellular ATP mediates mast cell-dependent intestinal inflammation through P2X7 purinoceptors. Nat Commun 3:1034
Bulanova E, Budagian V, Orinska Z, Koch-Nolte F, Haag F, Bulfone-Paus S (2009) ATP induces P2X7 receptor-independent cytokine and chemokine expression through P2X1 and P2X3 receptors in murine mast cells. J Leukoc Biol 85:692–702
Wareham K, Vial C, Wykes RC, Bradding P, Seward EP (2009) Functional evidence for the expression of P2X1, P2X4 and P2X7 receptors in human lung mast cells. Br J Pharmacol 157:1215–1224
Arandjelovic S, McKenney KR, Leming SS, Mowen KA (2012) ATP induces protein arginine deiminase 2-dependent citrullination in mast cells through the P2X7 purinergic receptor. J Immunol 189:4112–4122
Qian YX, McCloskey MA (1993) Activation of mast cell K+ channels through multiple G protein-linked receptors. Proc Natl Acad Sci U S A 90:7844–7848
Feng C, Mery AG, Beller EM, Favot C, Boyce JA (2004) Adenine nucleotides inhibit cytokine generation by human mast cells through a G s-coupled receptor. J Immunol 173:7539–7547
Gao ZG, Ding Y, Jacobson KA (2010) UDP-glucose acting at P2Y14 receptors is a mediator of mast cell degranulation. Biochem Pharmacol 79:873–879
Gao ZG, Wei Q, Jayasekara MP, Jacobson KA (2013) The role of P2Y14 and other P2Y receptors in degranulation of human LAD2 mast cells. Purinergic Signal 9:31–40
Haskó G, Szabó C (1998) Regulation of cytokine and chemokine production by transmitters and co-transmitters of the autonomic nervous system. Biochem Pharmacol 56:1079–1087
Burnstock G (2004) The Autonomic Neuroeffector Junction. In: Robertson D, Low P, Burnstock G, Biaggioni I (eds) Primer on the autonomic nervous system, 2nd edn. Elsevier, Amsterdam, pp 29–33
Burnstock G (2008) Non-synaptic transmission at autonomic neuroeffector junctions. Neurochem Int 52:14–25
Williams RM, Bienenstock J, Stead RH (1995) Mast cells: the neuroimmune connection. Chem Immunol 61:208–235
Kiernan JA (1974) Action of adenosine triphosphate on mast cells in normal and denervated skin. Arch Dermatol Forsch 251:83–86
Newson B, Dahlstrom A, Enerback L, Ahlman H (1983) Suggestive evidence for a direct innervation of mucosal mast cells. Neuroscience 10:565–570
Dimitriadou V, Aubineau P, Taxi J, Seylaz J (1987) Ultrastructural evidence for a functional unit between nerve fibers and type II cerebral mast cells in the cerebral vascular wall. Neuroscience 22:621–630
Levine JD, Coderre TJ, Covinsky K, Basbaum AI (1990) Neural influences on synovial mast cell density in rat. J Neurosci Res 26:301–307
Keller JT, Dimlich RV, Zuccarello M, Lanker L, Strauss TA, Fritts MJ (1991) Influence of the sympathetic nervous system as well as trigeminal sensory fibres on rat dural mast cells. Cephalalgia 11:215–221
Dimitriadou V, Rouleau A, Trung T, Newlands GJ, Miller HR, Luffau G, Schwartz JC, Garbarg M (1997) Functional relationships between sensory nerve fibers and mast cells of dura mater in normal and inflammatory conditions. Neuroscience 77:829–839
Gottwald TP, Hewlett BR, Lhotak S, Stead RH (1995) Electrical stimulation of the vagus nerve modulates the histamine content of mast cells in the rat jejunal mucosa. Neuroreport 7:313–317
Suzuki R, Furuno T, Okamoto K, Teshima R, Nakanishi M (2007) ATP plays a role in neurite stimulation with activated mast cells. J Neuroimmunol 192:49–56
Nakanishi M, Furuno T (2008) Molecular basis of neuroimmune interaction in an in vitro coculture approach. Cell Mol Immunol 5:249–259
Arizono N, Matsuda S, Hattori T, Kojima Y, Maeda T, Galli SJ (1990) Anatomical variation in mast cell nerve associations in the rat small intestine, heart, lung, and skin. Similarities of distances between neural processes and mast cells, eosinophils, or plasma cells in the jejunal lamina propria. Lab Invest 62:626–634
Chelmicka-Schorr E, Kwasniewski MN, Czlonkowska A (1992) Sympathetic nervous system modulates macrophage function. Int J Immunopharmacol 14:841–846
Madden KS, Moynihan JA, Brenner GJ, Felten SY, Felten DL (1994) Sympathetic nervous system modulation of the immune system. III. Alterations in T and B cell proliferation and differentiation in vitro following chemical sympathectomy. J Neuroimmunol 49:77–87
Crivellato E, Soldano F, Travan L, Fusaroli P, Mallardi F (1998) Apposition of enteric nerve fibers to plasma cells and immunoblasts in the mouse small bowel. Neurosci Lett 241:123–126
Genton L, Kudsk KA (2003) Interactions between the enteric nervous system and the immune system: role of neuropeptides and nutrition. Am J Surg 186:253–258
Lappin D, Whaley K (1981) Cyclic AMP-mediated modulation of the production of the second component of human complement by monocytes. Int Arch Allergy Appl Immunol 65:85–90
Lappin D, Whaley K (1984) Adenosine A2 receptors on human monocytes modulate C2 production. Clin Exp Immunol 57:454–460
Salmon JE, Brogle N, Brownlie C, Edberg JC, Kimberly RP, Chen BX, Erlanger BF (1993) Human mononuclear phagocytes express adenosine A1 receptors. A novel mechanism for differential regulation of Fcγ receptor function. J Immunol 151:2775–2785
Le Vraux V, Chen YL, Masson I, De Sousa M, Giroud JP, Florentin I, Chauvelot-Moachon L (1993) Inhibition of human monocyte TNF production by adenosine receptor agonists. Life Sci 52:1917–1924
Zhang JG, Hepburn L, Cruz G, Borman RA, Clark KL (2005) The role of adenosine A2A and A2B receptors in the regulation of TNF-α production by human monocytes. Biochem Pharmacol 69:883–889
Link AA, Kino T, Worth JA, McGuire JL, Crane ML, Chrousos GP, Wilder RL, Elenkov IJ (2000) Ligand-activation of the adenosine A2a receptors inhibits IL-12 production by human monocytes. J Immunol 164:436–442
Perez-Aso M, Feig JL, Aránzazu M, Cronstein BN (2013) Adenosine A2A receptor and TNF-α regulate the circadian machinery of the human monocytic THP-1 cells. Inflammation 36:152–162
Ramakers BP, Riksen NP, Rongen GA, van der Hoeven JG, Smits P, Pickkers P (2006) The effect of adenosine receptor agonists on cytokine release by human mononuclear cells depends on the specific Toll-like receptor subtype used for stimulation. Cytokine 35:95–99
Takahashi HK, Kanke T, Liu K, Yoshino T, Sendo T, Tanaka N, Nishibori M (2007) Adenosine A2A-receptor stimulation inhibits lipopolysaccharide-induced interleukin-18 production in monocytes. J Pharmacol Sci 104:183–186
Hamano R, Takahashi HK, Iwagaki H, Kanke T, Liu K, Yoshino T, Sendo T, Nishibori M, Tanaka N (2008) Stimulation of adenosine A2A receptor inhibits LPS-induced expression of intercellular adhesion molecule 1 and production of TNF-α in human peripheral blood mononuclear cells. Shock 29:154–159
Merrill JT, Shen C, Schreibman D, Coffey D, Zakharenko O, Fisher R, Lahita RG, Salmon J, Cronstein BN (1997) Adenosine A1 receptor promotion of multinucleated giant cell formation by human monocytes: a mechanism for methotrexate-induced nodulosis in rheumatoid arthritis. Arthritis Rheum 40:1308–1315
Barbieri D, Abbracchio MP, Salvioli S, Monti D, Cossarizza A, Ceruti S, Brambilla R, Cattabeni F, Jacobson KA, Franceschi C (1998) Apoptosis by 2-chloro-2'-deoxy-adenosine and 2-chloro-adenosine in human peripheral blood mononuclear cells. Neurochem Int 32:493–504
Altieri DC, Wiltse WL, Edgington TS (1990) Signal transduction initiated by extracellular nucleotides regulates the high affinity ligand recognition of the adhesive receptor CD11b/CD18. J Immunol 145:662–670
Ventura MA, Thomopoulos P (1995) ADP and ATP activate distinct signaling pathways in human promonocytic U-937 cells differentiated with 1,25-dihydroxy-vitamin D3. Mol Pharmacol 47:104–114
Humphreys BD, Dubyak GR (1996) Induction of the P2z/P2X7 nucleotide receptor and associated phospholipase D activity by lipopolysaccharide and IFN-γ in the human THP-1 monocytic cell line. J Immunol 157:5627–5637
Rassendren F, Buell GN, Virginio C, Collo G, North RA, Surprenant A (1997) The permeabilizing ATP receptor, P2X7. Cloning and expression of a human cDNA. J Biol Chem 272:5482–5486
Aga M, Johnson CJ, Hart AP, Guadarrama AG, Suresh M, Svaren J, Bertics PJ, Darien BJ (2002) Modulation of monocyte signalling and pore formation in response to agonists of the nucleotide receptor P2X7. J Leukoc Biol 72:222–232
Humphreys BD, Dubyak GR (1998) Modulation of P2X7 nucleotide receptor expression by pro- and anti-inflammatory stimuli in THP-1 monocytes. J Leukoc Biol 64:265–273
Grahames CB, Michel AD, Chessell IP, Humphrey PP (1999) Pharmacological characterization of ATP- and LPS-induced IL-1β release in human monocytes. Br J Pharmacol 127:1915–1921
Warren AY, Harvey L, Shaw RW, Khan RN (2008) Interleukin-1β secretion from cord blood mononuclear cells in vitro involves P2X7 receptor activation. Reprod Sci 15:189–194
Jalilian I, Peranec M, Curtis BL, Seavers A, Spildrejorde M, Sluyter V, Sluyter R (2012) Activation of the damage-associated molecular pattern receptor P2X7 induces interleukin-1β release from canine monocytes. Vet Immunol Immunopathol 149:86–91
Mehta VB, Hart J, Wewers MD (2001) ATP-stimulated release of interleukin (IL)-1β and IL-18 requires priming by lipopolysaccharide and is independent of caspase-1 cleavage. J Biol Chem 276:3820–3826
Gardella S, Andrei C, Ferrera D, Lotti LV, Torrisi MR, Bianchi ME, Rubartelli A (2002) The nuclear protein HMGB1 is secreted by monocytes via a non-classical, vesicle-mediated secretory pathway. EMBO Rep 3:995–1001
Piccini A, Carta S, Tassi S, Lasiglié D, Fossati G, Rubartelli A (2008) ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1β and IL-18 secretion in an autocrine way. Proc Natl Acad Sci U S A 105:8067–8072
Asgari E, Le Friec G, Yamamoto H, Perucha E, Sacks SS, Köhl J, Cook HT, Kemper C (2013) C3a modulates IL-1β secretion in human monocytes by regulating ATP efflux and subsequent NLRP3 inflammasome activation. Blood 122:3473–3481
Di Virgilio F (2007) Liaisons dangereuses: P2X7 and the inflammasome. Trends Pharmacol Sci 28:465–472
Sluyter R, Shemon AN, Wiley JS (2004) Glu496 to Ala polymorphism in the P2X7 receptor impairs ATP-induced IL-1β release from human monocytes. J Immunol 172:3399–3405
Straub RH, Mayer M, Kreutz M, Leeb S, Schölmerich J, Falk W (2000) Neurotransmitters of the sympathetic nerve terminal are powerful chemoattractants for monocytes. J Leukoc Biol 67:553–558
Kaufmann A, Musset B, Limberg SH, Renigunta V, Sus R, Dalpke AH, Heeg KM, Robaye B, Hanley PJ (2005) "Host tissue damage" signal ATP promotes non-directional migration and negatively regulates toll-like receptor signaling in human monocytes. J Biol Chem 280:32459–32467
Akbar GK, Mills DC, Kunapuli SP (1997) Characterization of extracellular nucleotide-induced Mac-1 (αMβ2 integrin) surface expression on peripheral blood leukocytes. Biochem Biophys Res Commun 233:71–75
Warny M, Aboudola S, Robson SC, Sévigny J, Communi D, Soltoff SP, Kelly CP (2001) P2Y6 nucleotide receptor mediates monocyte interleukin-8 production in response to UDP or lipopolysaccharide. J Biol Chem 276:26051–26056
Ben Yebdri F, Kukulski F, Tremblay A, Sévigny J (2009) Concomitant activation of P2Y2 and P2Y6 receptors on monocytes is required for TLR1/2-induced neutrophil migration by regulating IL-8 secretion. Eur J Immunol 39:2885–2894
Rizzo R, Ferrari D, Melchiorri L, Stignani M, Gulinelli S, Baricordi OR, Di Virgilio F (2009) Extracellular ATP acting at the P2X7 receptor inhibits secretion of soluble HLA-G from human monocytes. J Immunol 183:4302–4311
Hill LM, Gavala ML, Lenertz LY, Bertics PJ (2010) Extracellular ATP may contribute to tissue repair by rapidly stimulating purinergic receptor X7-dependent vascular endothelial growth factor release from primary human monocytes. J Immunol 185:3028–3034
Gu BJ, Saunders BM, Jursik C, Wiley JS (2010) The P2X7-nonmuscle myosin membrane complex regulates phagocytosis of nonopsonized particles and bacteria by a pathway attenuated by extracellular ATP. Blood 115:1621–1631
Aksamit RR, Backlund PS Jr, Cantoni GL (1983) Chemotaxis and the synthesis of specific proteins are inhibited by 3-deazaadenosine and other adenosine analogs in a mouse macrophage cell line. J Biol Chem 258:20–23
Riches DW, Watkins JL, Henson PM, Stanworth DR (1985) Regulation of macrophage lysosomal secretion by adenosine, adenosine phosphate esters, and related structural analogues of adenosine. J Leukoc Biol 37:545–557
McWhinney CD, Dudley MW, Bowlin TL, Peet NP, Schook L, Bradshaw M, De M, Borcherding DR, Edwards CK III (1996) Activation of adenosine A3 receptors on macrophages inhibits tumor necrosis factor-α. Eur J Pharmacol 310:209–216
Németh ZH, Leibovich SJ, Deitch EA, Vizi ES, Szabó C, Haskó G (2003) cDNA microarray analysis reveals a nuclear factor-κB-independent regulation of macrophage function by adenosine. J Pharmacol Exp Ther 306:1042–1049
Hon WM, Moochhala S, Khoo HE (1997) Adenosine and its receptor agonists potentiate nitric oxide synthase expression induced by lipopolysaccharide in RAW 264.7 murine macrophages. Life Sci 60:1327–1335
Zídek Z, Kmoníckova E, Holy A (2004) Involvement of adenosine A1 receptors in upregulation of nitric oxide by acyclic nucleotide analogues. Eur J Pharmacol 501:79–86
Xaus J, Mirabet M, Lloberas J, Soler C, Lluis C, Franco R, Celada A (1999) IFN-γ up-regulates the A2B adenosine receptor expression in macrophages: a mechanism of macrophage deactivation. J Immunol 162:3607–3614
Murphree LJ, Sullivan GW, Marshall MA, Linden J (2005) Lipopolysaccharide rapidly modifies adenosine receptor transcripts in murine and human macrophages: role of NF-κB in A2A adenosine receptor induction. Biochem J 391:575–580
Elson G, Eisenberg M, Garg C, Outram S, Ferrante CJ, Hasko G, Leibovich SJ (2013) Induction of murine adenosine A2A receptor expression by LPS: analysis of the 5' upstream promoter. Genes Immun 14:147–153
Kreckler LM, Wan TC, Ge ZD, Auchampach JA (2006) Adenosine inhibits tumor necrosis factor-α release from mouse peritoneal macrophages via A2A and A2B but not the A3 adenosine receptor. J Pharmacol Exp Ther 317:172–180
Ezeamuzie CI, Khan I (2007) The role of adenosine A2 receptors in the regulation of TNF-α production and PGE2 release in mouse peritoneal macrophages. Int Immunopharmacol 7:483–490
Chen H, Yang D, Carroll SH, Eltzschig HK, Ravid K (2009) Activation of the macrophage A2b adenosine receptor regulates tumor necrosis factor-α levels following vascular injury. Exp Hematol 37:533–538
Buenestado A, Grassin Delyle S, Arnould I, Besnard F, Naline E, Blouquit-Laye S, Chapelier A, Bellamy JF, Devillier P (2010) The role of adenosine receptors in regulating production of tumour necrosis factor-alpha and chemokines by human lung macrophages. Br J Pharmacol 159:1304–1311
Németh ZH, Lutz CS, Csóka B, Deitch EA, Leibovich SJ, Gause WC, Tone M, Pacher P, Vizi ES, Haskó G (2005) Adenosine augments IL-10 production by macrophages through an A2B receptor-mediated posttranscriptional mechanism. J Immunol 175:8260–8270
Csóka B, Németh ZH, Selmeczy Z, Koscsó B, Pacher P, Vizi ES, Deitch EA, Haskó G (2007) Role of A2A adenosine receptors in regulation of opsonized E. coli-induced macrophage function. Purinergic Signal 3:447–452
Csóka B, Németh ZH, Virág L, Gergely P, Leibovich SJ, Pacher P, Sun CX, Blackburn MR, Vizi ES, Deitch EA, Haskó G (2007) A2A adenosine receptors and C/EBPβ are crucially required for IL-10 production by macrophages exposed to Escherichia coli. Blood 110:2685–2695
Zanin RF, Braganhol E, Bergamin LS, Campesato LF, Filho AZ, Moreira JC, Morrone FB, Sévigny J, Schetinger MR, de Souza Wyse AT, Battastini AM (2012) Differential macrophage activation alters the expression profile of NTPDase and ecto-5'-nucleotidase. PLoS One 7:e31205
Soledade CS, Franchini KG, Linden J, Huo Y (2007) Stimulation of adenosine A2A receptor regulates peroxisome proliferator activated receptors in macrophages. FASEB J 21:A1035
De Ponti C, Carini R, Alchera E, Nitti MP, Locati M, Albano E, Cairo G, Tacchini L (2007) Adenosine A2a receptor-mediated, normoxic induction of HIF-1 through PKC and PI-3 K-dependent pathways in macrophages. J Leukoc Biol 82:392–402
Leibovich SJ, Chen JF, Pinhal-Enfield G, Belem PC, Elson G, Rosania A, Ramanathan M, Montesinos C, Jacobson M, Schwarzschild MA, Fink JS, Cronstein B (2002) Synergistic up-regulation of vascular endothelial growth factor expression in murine macrophages by adenosine A2A receptor agonists and endotoxin. Am J Pathol 160:2231–2244
Ernens I, Leonard F, Vausort M, Rolland-Turner M, Devaux Y, Wagner DR (2010) Adenosine up-regulates vascular endothelial growth factor in human macrophages. Biochem Biophys Res Commun 392:351–356
Velot E, Haas B, Leonard F, Ernens I, Rolland-Turner M, Schwartz C, Longrois D, Devaux Y, Wagner DR (2008) Activation of the adenosine-A3 receptor stimulates matrix metalloproteinase-9 secretion by macrophages. Cardiovasc Res 80:246–254
Barczyk K, Ehrchen J, Tenbrock K, Ahlmann M, Kneidl J, Viemann D, Roth J (2010) Glucocorticoids promote survival of anti-inflammatory macrophages via stimulation of adenosine receptor A3. Blood 116:446–455
Steinberg TH, Newman AS, Swanson JA, Silverstein SC (1987) ATP4− permeabilizes the plasma membrane of mouse macrophages to fluorescent dyes. J Biol Chem 262:8884–8888
Buisman HP, Steinberg TH, Fischbarg J, Silverstein SC, Vogelzang SA, Ince C, Ypey DL, Leijh PC (1988) Extracellular ATP induces a large nonselective conductance in macrophage plasma membranes. Proc Natl Acad Sci U S A 85:7988–7992
Steinberg TH, Silverstein SC (1987) Extracellular ATP4− promotes cation fluxes in the J774 mouse macrophage cell line. J Biol Chem 262:3118–3122
Greenberg S, Di Virgilio F, Steinberg TH, Silverstein SC (1988) Extracellular nucleotides mediate Ca2+ fluxes in J774 macrophages by two distinct mechanisms. J Biol Chem 263:10337–10343
Coutinho-Silva R, Alves LA, Savino W, Persechini PM (1996) A cation non-selective channel induced by extracellular ATP in macrophages and phagocytic cells of the thymic reticulum. Biochim Biophys Acta 1278:125–130
Nakanishi M, Takihara H, Minoru Y, Yagawa K (1991) Extracellular ATP itself elicits superoxide generation in guinea pig peritoneal macrophages. FEBS Lett 282:91–94
Murphy JK, Livingston FR, Gozal E, Torres M, Forman HJ (1993) Stimulation of the rat alveolar macrophage respiratory burst by extracellular adenine nucleotides. Am J Respir Cell Mol Biol 9:505–510
Sung SS, Young JD, Origlio AM, Heiple JM, Kaback HR, Silverstein SC (1985) Extracellular ATP perturbs transmembrane ion fluxes, elevates cytosolic [Ca2+], and inhibits phagocytosis in mouse macrophages. J Biol Chem 260:13442–13449
Murgia M, Pizzo P, Steinberg TH, Di Virgilio F (1992) Characterization of the cytotoxic effect of extracellular ATP in J774 mouse macrophages. Biochem J 288:897–901
Blanchard DK, McMillen S, Djeu JY (1991) IFN-γ enhances sensitivity of human macrophages to extracellular ATP-mediated lysis. J Immunol 147:2579–2585
Pfeilschifter J, Thüring B, Festa F (1989) Extracellular ATP stimulates poly(inositol phospholipid) hydrolysis and eicosanoid synthesis in mouse peritoneal macrophages in culture. Eur J Biochem 186:509–513
Murgia M, Hanau S, Pizzo P, Rippa M, Di Virgilio F (1993) Oxidized ATP. An irreversible inhibitor of the macrophage purinergic P2Z receptor. J Biol Chem 268:8199–8203
el-Moatassim C, Dubyak GR (1993) Dissociation of the pore-forming and phospholipase D activities stimulated via P2z purinergic receptors in BAC1.2 F5 macrophages. Product inhibition of phospholipase D enzyme activity. J Biol Chem 268:15571–15578
Hickman SE, El Khoury J, Greenberg S, Schieren I, Silverstein SC (1994) P2Z adenosine triphosphate receptor activity in cultured human monocyte-derived macrophages. Blood 84:2452–2456
Falzoni S, Munerati M, Ferrari D, Spisani S, Moretti S, Di Virgilio F (1995) The purinergic P2Z receptor of human macrophage cells. Characterization and possible physiological role. J Clin Invest 95:1207–1216
Perregaux D, Gabel CA (1994) Interleukin-1β maturation and release in response to ATP and nigericin. Evidence that potassium depletion mediated by these agents is a necessary and common feature of their activity. J Biol Chem 269:15195–15203
Griffiths RJ, Stam EJ, Downs JT, Otterness IG (1995) ATP induces the release of IL-1 from LPS-primed cells in vivo. J Immunol 154:2821–2828
Ferrari D, Chiozzi P, Falzoni S, dal Susino M, Melchiorri L, Baricordi OR, Di Virgilio F (1997) Extracellular ATP triggers IL-1β release by activating the purinergic P2Z receptor of human macrophages. J Immunol 159:1451–1458
Brough D, Le Feuvre RA, Wheeler RD, Solovyova N, Hilfiker S, Rothwell NJ, Verkhratsky A (2003) Ca2+ stores and Ca2+ entry differentially contribute to the release of IL-1β and IL-1α from murine macrophages. J Immunol 170:3029–3036
Qu Y, Franchi L, Nunez G, Dubyak GR (2007) Nonclassical IL-1β secretion stimulated by P2X7 receptors is dependent on inflammasome activation and correlated with exosome release in murine macrophages. J Immunol 179:1913–1925
Pelegrin P, Barroso-Gutierrez C, Surprenant A (2008) P2X7 receptor differentially couples to distinct release pathways for IL-1β in mouse macrophage. J Immunol 180:7147–7157
Lee BH, Hwang DM, Palaniyar N, Grinstein S, Philpott DJ, Hu J (2012) Activation of P2X7 receptor by ATP plays an important role in regulating inflammatory responses during acute viral infection. PLoS One 7:e35812
Petrovski G, Ayna G, Majai G, Hodrea J, Benko S, Mádi A, Fésüs L (2011) Phagocytosis of cells dying through autophagy induces inflammasome activation and IL-1β release in human macrophages. Autophagy 7:321–330
Niemi K, Teirilä L, Lappalainen J, Rajamäki K, Baumann MH, Öörni K, Wolff H, Kovanen PT, Matikainen S, Eklund KK (2011) Serum amyloid A activates the NLRP3 inflammasome via P2X7 receptor and a cathepsin B-sensitive pathway. J Immunol 186:6119–6128
Lucattelli M, Cicko S, Muller T, Lommatzsch M, De Cunto G, Cardini S, Sundas W, Grimm M, Zeiser R, Durk T, Zissel G, Sorichter S, Ferrari D, Di Virgilio F, Virchow JC, Lungarella G, Idzko M (2011) P2X7 receptor signaling in the pathogenesis of smoke-induced lung inflammation and emphysema. Am J Respir Cell Mol Biol 44:423–429
Lammas DA, Stober C, Harvey CJ, Kendrick N, Panchalingam S, Kumararatne DS (1997) ATP-induced killing of mycobacteria by human macrophages is mediated by purinergic P2Z (P2X7) receptors. Immunity 7:433–444
Kusner DJ, Barton JA (2001) ATP stimulates human macrophages to kill intracellular virulent Mycobacterium tuberculosis via calcium-dependent phagosome-lysosome fusion. J Immunol 167:3308–3315
Kusner DJ, Adams J (2000) ATP-induced killing of virulent Mycobacterium tuberculosis within human macrophages requires phospholipase D. J Immunol 164:379–388
Fairbairn IP, Stober CB, Kumararatne DS, Lammas DA (2001) ATP-mediated killing of intracellular mycobacteria by macrophages is a P2X 7-dependent process inducing bacterial death by phagosome-lysosome fusion. J Immunol 167:3300–3307
Placido R, Auricchio G, Falzoni S, Battistini L, Colizzi V, Brunetti E, Di Virgilio F, Mancino G (2006) P2X7 purinergic receptors and extracellular ATP mediate apoptosis of human monocytes/macrophages infected with Mycobacterium tuberculosis reducing the intracellular bacterial viability. Cell Immunol 244:10–18
Biswas D, Qureshi OS, Lee WY, Croudace JE, Mura M, Lammas DA (2008) ATP-induced autophagy is associated with rapid killing of intracellular mycobacteria within human monocytes/macrophages. BMC Immunol 9:35
Saunders BM, Fernando SL, Sluyter R, Britton WJ, Wiley JS (2003) A loss-of-function polymorphism in the human P2X7 receptor abolishes ATP-mediated killing of mycobacteria. J Immunol 171:5442–5446
Fernando SL, Saunders BM, Sluyter R, Skarratt KK, Wiley JS, Britton WJ (2005) Gene dosage determines the negative effects of polymorphic alleles of the P2X7 receptor on adenosine triphosphate-mediated killing of mycobacteria by human macrophages. J Infect Dis 192:149–155
Shemon AN, Sluyter R, Fernando SL, Clarke AL, Dao-Ung LP, Skarratt KK, Saunders BM, Tan KS, Gu BJ, Fuller SJ, Britton WJ, Petrou S, Wiley JS (2006) A Thr357 to Ser polymorphism in homozygous and compound heterozygous subjects causes absent or reduced P2X7 function and impairs ATP-induced mycobacterial killing by macrophages. J Biol Chem 281:2079–2086
Franco-Martínez S, Niño-Moreno P, Bernal-Silva S, Baranda L, Rocha-Meza M, Portales-Cervantes L, Layseca-Espinosa E, González-Amaro R, Portales-Pérez D (2006) Expression and function of the purinergic receptor P2X7 in patients with pulmonary tuberculosis. Clin Exp Immunol 146:253–261
Chaves SP, Torres-Santos EC, Marques C, Figliuolo VR, Persechini PM, Coutinho-Silva R, Rossi-Bergmann B (2009) Modulation of P2X7 purinergic receptor in macrophages by Leishmania amazonensis and its role in parasite elimination. Microbes Infect 11:842–849
Chaves MM, Marques-da-Silva C, Monteiro AP, Canetti C, Coutinho-Silva R (2014) Leukotriene B4 modulates P2X7 receptor-mediated Leishmania amazonensis elimination in murine macrophages. J Immunol 192:4765–4773
Corrêa G, Marques da Silva C, de Abreu Moreira-Souza AC, Vommaro RC, Coutinho-Silva R (2010) Activation of the P2X7 receptor triggers the elimination of Toxoplasma gondii tachyzoites from infected macrophages. Microbes Infect 12:497–504
Lees MP, Fuller SJ, McLeod R, Boulter NR, Miller CM, Zakrzewski AM, Mui EJ, Witola WH, Coyne JJ, Hargrave AC, Jamieson SE, Blackwell JM, Wiley JS, Smith NC (2010) P2X7 receptor-mediated killing of an intracellular parasite, Toxoplasma gondii, by human and murine macrophages. J Immunol 184:7040–7046
Tonetti M, Sturla L, Bistolfi T, Benatti U, De Flora A (1994) Extracellular ATP potentiates nitric oxide synthase expression induced by lipopolysaccharide in RAW 264.7 murine macrophages. Biochem Biophys Res Commun 203:430–435
Tonetti M, Sturla L, Giovine M, Benatti U, De Flora A (1995) Extracellular ATP enhances mRNA levels of nitric oxide synthase and TNF-α in lipopolysaccharide-treated RAW 264.7 murine macrophages. Biochem Biophys Res Commun 214:125–130
Denlinger LC, Fisette PL, Garis KA, Kwon G, Vazquez-Torres A, Simon AD, Nguyen B, Proctor RA, Bertics PJ, Corbett JA (1996) Regulation of inducible nitric oxide synthase expression by macrophage purinoreceptors and calcium. J Biol Chem 271:337–342
Hu Y, Fisette PL, Denlinger LC, Guadarrama AG, Sommer JA, Proctor RA, Bertics PJ (1998) Purinergic receptor modulation of lipopolysaccharide signaling and inducible nitric-oxide synthase expression in RAW 264.7 macrophages. J Biol Chem 273:27170–27175
Sperlágh B, Haskó G, Németh Z, Vizi ES (1998) ATP released by LPS increases nitric oxide production in raw 264.7 macrophage cell line via P2Z/P2X7 receptors. Neurochem Int 33:209–215
Sommer JA, Fisette PL, Hu Y, Denlinger LC, Guerra AN, Bertics PJ, Proctor RA (1999) Purinergic receptor modulation of LPS-stimulated signaling events and nitric oxide release in RAW 264.7 macrophages. J Endotoxin Res 5:70–74
Chen YJ, Hsu KW, Chen YL (2006) Acute glucose overload potentiates nitric oxide production in lipopolysaccharide-stimulated macrophages: the role of purinergic receptor activation. Cell Biol Int 30:817–822
Pfeiffer ZA, Guerra AN, Hill LM, Gavala ML, Prabhu U, Aga M, Hall DJ, Bertics PJ (2007) Nucleotide receptor signaling in murine macrophages is linked to reactive oxygen species generation. Free Radic Biol Med 42:1506–1516
Cruz CM, Rinna A, Forman HJ, Ventura AL, Persechini PM, Ojcius DM (2007) ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. J Biol Chem 282:2871–2879
Lenertz LY, Gavala ML, Hill LM, Bertics PJ (2009) Cell signaling via the P2X7 nucleotide receptor: linkage to ROS production, gene transcription, and receptor trafficking. Purinergic Signal 5:175–187
Costa-Junior HM, Mendes AN, Davis GH, da Cruz CM, Ventura AL, Serezani CH, Faccioli LH, Nomizo A, Freire-de-Lima CG, Bisaggio RC, Persechini PM (2009) ATP-induced apoptosis involves a Ca2+-independent phospholipase A2 and 5-lipoxygenase in macrophages. Prostaglandins Other Lipid Mediat 88:51–61
Moore SF, MacKenzie AB (2007) Murine macrophage P2X7 receptors support rapid prothrombotic responses. Cell Signal 19:855–866
Furlan-Freguia C, Marchese P, Gruber A, Ruggeri ZM, Ruf W (2011) P2X7 receptor signaling contributes to tissue factor-dependent thrombosis in mice. J Clin Invest 121:2932–2944
Gu BJ, Duce JA, Valova VA, Wong B, Bush AI, Petrou S, Wiley JS (2012) P2X7 receptor-mediated scavenger activity of mononuclear phagocytes toward non-opsonized particles and apoptotic cells is inhibited by serum glycoproteins but remains active in cerebrospinal fluid. J Biol Chem 287:17318–17330
Gu BJ, Baird PN, Vessey KA, Skarratt KK, Fletcher EL, Fuller SJ, Richardson AJ, Guymer RH, Wiley JS (2013) A rare functional haplotype of the P2RX4 and P2RX7 genes leads to loss of innate phagocytosis and confers increased risk of age-related macular degeneration. FASEB J 27:1479–1487
Di Virgilio F, Falzoni S, Chiozzi P, Sanz JM, Ferrari D, Buell GN (1999) ATP receptors and giant cell formation. J Leukoc Biol 66:723–726
Chiozzi P, Sanz JM, Ferrari D, Falzoni S, Aleotti A, Buell GN, Collo G, Di Virgilio F (1997) Spontaneous cell fusion in macrophage cultures expressing high levels of the P2Z/P2X7 receptor. J Cell Biol 138:697–706
Lemaire I, Falzoni S, Leduc N, Zhang B, Pellegatti P, Adinolfi E, Chiozzi P, Di Virgilio F (2006) Involvement of the purinergic P2X7 receptor in the formation of multinucleated giant cells. J Immunol 177:7257–7265
Lemaire I, Falzoni S, Zhang B, Pellegatti P, Di Virgilio F (2011) The P2X7 receptor and Pannexin-1 are both required for the promotion of multinucleated macrophages by the inflammatory cytokine GM-CSF. J Immunol 187:3878–3887
Coutinho-Silva R, Ojcius DC, Gorecki DC, Persechini PM, Bisaggio RC, Dunn PM, Burnstock G (2005) Multiple P2X and P2Y receptor subtypes in mouse J774, spleen and peritoneal macrophages. Biochem Pharmacol 69:641–655
Myrtek D, Müller T, Geyer V, Derr N, Ferrari D, Zissel G, Dürk T, Sorichter S, Luttmann W, Kuepper M, Norgauer J, Di Virgilio F, Virchow JC Jr, Idzko M (2008) Activation of human alveolar macrophages via P2 receptors: coupling to intracellular Ca2+ increases and cytokine secretion. J Immunol 181:2181–2188
Eschke D, Wüst M, Hauschildt S, Nieber K (2002) Pharmacological characterization of the P2X7 receptor on human macrophages using the patch-clamp technique. Naunyn Schmiedebergs Arch Pharmacol 365:168–171
Brône B, Moechars D, Marrannes R, Mercken M, Meert T (2007) P2X currents in peritoneal macrophages of wild type and P2X4 −/− mice. Immunol Lett 113:83–89
Kawano A, Tsukimoto M, Mori D, Noguchi T, Harada H, Takenouchi T, Kitani H, Kojima S (2012) Regulation of P2X7-dependent inflammatory functions by P2X4 receptor in mouse macrophages. Biochem Biophys Res Commun 420:102–107
Kawano A, Tsukimoto M, Noguchi T, Hotta N, Harada H, Takenouchi T, Kitani H, Kojima S (2012) Involvement of P2X4 receptor in P2X7 receptor-dependent cell death of mouse macrophages. Biochem Biophys Res Commun 419:374–380
Hazleton JE, Berman JW, Eugenin EA (2012) Purinergic receptors are required for HIV-1 infection of primary human macrophages. J Immunol 188:4488–4495
Hanley PJ, Musset B, Renigunta V, Limberg SH, Dalpke AH, Sus R, Heeg KM, Preisig-Müller R, Daut J (2004) Extracellular ATP induces oscillations of intracellular Ca2+ and membrane potential and promotes transcription of IL-6 in macrophages. Proc Natl Acad Sci U S A 101:9479–9484
del Rey A, Renigunta V, Dalpke AH, Leipziger J, Matos JE, Robaye B, Zuzarte M, Kavelaars A, Hanley PJ (2006) Knock-out mice reveal the contributions of P2Y and P2X receptors to nucleotide-induced Ca2+ signaling in macrophages. J Biol Chem 281:35147–35155
Qu Y, Misaghi S, Newton K, Gilmour LL, Louie S, Cupp JE, Dubyak GR, Hackos D, Dixit VM (2011) Pannexin-1 is required for ATP release during apoptosis but not for inflammasome activation. J Immunol 186:6553–6561
Kronlage M, Song J, Sorokin L, Isfort K, Schwerdtle T, Leipziger J, Robaye B, Conley PB, Kim HC, Sargin S, Schön P, Schwab A, Hanley PJ (2010) Autocrine purinergic receptor signaling is essential for macrophage chemotaxis. Sci Signal 3:ra55
Chen BC, Chou CF, Lin WW (1998) Pyrimidinoceptor-mediated potentiation of inducible nitric-oxide synthase induction in J774 macrophages. Role of intracellular calcium. J Biol Chem 273:29754–29763
Chen BC, Lin WW (2000) Pyrimidinoceptor potentiation of macrophage PGE2 release involved in the induction of nitric oxide synthase. Br J Pharmacol 130:777–786
Stokes L, Surprenant A (2007) Purinergic P2Y2 receptors induce increased MCP-1/CCL2 synthesis and release from rat alveolar and peritoneal macrophages. J Immunol 179:6016–6023
Eun SY, Seo J, Park SW, Lee JH, Chang KC, Kim HJ (2014) LPS potentiates nucleotide-induced inflammatory gene expression in macrophages via the upregulation of P2Y2 receptor. Int Immunopharmacol 18:270–276
Bar I, Guns PJ, Metallo J, Cammarata D, Wilkin F, Boeynams JM, Bult H, Robaye B (2008) Knockout mice reveal a role for P2Y6 receptor in macrophages, endothelial cells, and vascular smooth muscle cells. Mol Pharmacol 74:777–784
Zhang Z, Wang Z, Ren H, Yue M, Huang K, Gu H, Liu M, Du B, Qian M (2011) P2Y6 agonist uridine 5'-diphosphate promotes host defense against bacterial infection via monocyte chemoattractant protein-1-mediated monocytes/macrophages recruitment. J Immunol 186:5376–5387
Sakaki H, Tsukimoto M, Harada H, Moriyama Y, Kojima S (2013) Autocrine regulation of macrophage activation via exocytosis of ATP and activation of P2Y11 receptor. PLoS One 8:e59778
Parkinson FE, Paterson AR, Young JD, Cass CE (1993) Inhibitory effects of propentofylline on [3H]adenosine influx. A study of three nucleoside transport systems. Biochem Pharmacol 46:891–896
Banati RB, Schubert P, Rothe G, Gehrmann J, Rudolphi K, Valet G, Kreutzberg GW (1994) Modulation of intracellular formation of reactive oxygen intermediates in peritoneal macrophages and microglia/brain macrophages by propentofylline. J Cereb Blood Flow Metab 14:145–149
Schubert P, Rudolphi KA, Fredholm BB, Nakamura Y (1994) Modulation of nerve and glial function by adenosine - role in the development of ischemic damage. Int J Biochem 26:1227–1236
McRae A, Rudolphi KA, Schubert P (1994) Propentosylline depresses amyloid and Alzheimer's CSF microglial antigens after ischaemia. Neuroreport 5:1193–1196
McRae A, Ling EA, Schubert P, Rudolphi K (1998) Properties of activated microglia and pharmacologic interference by propentofylline. Alzheimer Dis Assoc Disord 12(Suppl 2):S15–S20
Schubert P, Ogata T, Rudolphi K, Marchini C, McRae A, Ferroni S (1997) Support of homeostatic glial cell signaling: a novel therapeutic approach by propentofylline. Ann N Y Acad Sci 826:337–347
Tsutsui S, Schnermann J, Noorbakhsh F, Henry S, Yong VW, Winston BW, Warren K, Power C (2004) A1 adenosine receptor upregulation and activation attenuates neuroinflammation and demyelination in a model of multiple sclerosis. J Neurosci 24:1521–1529
Färber K, Markworth S, Pannasch U, Nolte C, Prinz V, Kronenberg G, Gertz K, Endres M, Bechmann I, Enjyoji K, Robson SC, Kettenmann H (2008) The ectonucleotidase cd39/ENTPDase1 modulates purinergic-mediated microglial migration. Glia 56:331–341
Ohsawa K, Sanagi T, Nakamura Y, Suzuki E, Inoue K, Kohsaka S (2012) Adenosine A3 receptor is involved in ADP-induced microglial process extension and migration. J Neurochem 121:217–227
Orr AG, Orr AL, Li XJ, Gross RE, Traynelis SF (2009) Adenosine A2A receptor mediates microglial process retraction. Nat Neurosci 12:872–878
Yao SQ, Li ZZ, Huang QY, Li F, Wang ZW, Augusto E, He JC, Wang XT, Chen JF, Zheng RY (2012) Genetic inactivation of the adenosine A2A receptor exacerbates brain damage in mice with experimental autoimmune encephalomyelitis. J Neurochem 123:100–112
Kettenmann H, Banati R, Walz W (1993) Electrophysiological behavior of microglia. Glia 7:93–101
Walz W, Ilschner S, Ohlemeyer C, Banati R, Kettenmann H (1993) Extracellular ATP activates a cation conductance and a K+ conductance in cultured microglial cells from mouse brain. J Neurosci 13:4403–4411
Langosch JM, Gebicke-Haerter PJ, Nörenberg W, Illes P (1994) Characterization and transduction mechanisms of purinoceptors in activated rat microglia. Br J Pharmacol 113:29–34
Nörenberg W, Langosch JM, Gebicke-Haerter PJ, Illes P (1994) Characterization and possible function of adenosine 5'-triphosphate receptors in activated rat microglia. Br J Pharmacol 111:942–950
Ferrari D, Villalba M, Chiozzi P, Falzoni S, Ricciardi-Castagnoli P, Di Virgilio F (1996) Mouse microglial cells express a plasma membrane pore gated by extracellular ATP. J Immunol 156:1531–1539
Ferrari D, Chiozzi P, Falzoni S, Hanau S, Di Virgilio F (1997) Purinergic modulation of interleukin-1β release from microglial cells stimulated with bacterial endotoxin. J Exp Med 185:579–582
Brough D, Le Feuvre RA, Iwakura Y, Rothwell NJ (2002) Purinergic (P2X7) receptor activation of microglia induces cell death via an interleukin-1-independent mechanism. Mol Cell Neurosci 19:272–280
Skaper SD, Facci L, Culbert AA, Evans NA, Chessell I, Davis JB, Richardson JC (2006) P2X7 receptors on microglial cells mediate injury to cortical neurons in vitro. Glia 54:234–242
Sanz JM, Chiozzi P, Ferrari D, Colaianna M, Idzko M, Falzoni S, Fellin R, Trabace L, Di Virgilio F (2009) Activation of microglia by amyloid β requires P2X7 receptor expression. J Immunol 182:4378–4385
Tsuda M, Shigemoto-Mogami Y, Koizumi S, Mizokoshi A, Kohsaka S, Salter MW, Inoue K (2003) P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 424:778–783
Ohsawa K, Irino Y, Nakamura Y, Akazawa C, Inoue K, Kohsaka S (2007) Involvement of P2X4 and P2Y12 receptors in ATP-induced microglial chemotaxis. Glia 55:604–616
Haynes SE, Hollopeter G, Yang G, Kurpius D, Dailey ME, Gan WB, Julius D (2006) The P2Y12 receptor regulates microglial activation by extracellular nucleotides. Nat Neurosci 9:1512–1519
Koizumi S, Shigemoto-Mogami Y, Nasu-Tada K, Shinozaki Y, Ohsawa K, Tsuda M, Joshi BV, Jacobson KA, Kohsaka S, Inoue K (2007) UDP acting at P2Y6 receptors is a mediator of microglial phagocytosis. Nature 446:1091–1095
Inoue K, Koizumi S, Kataoka A, Tozaki-Saitoh H, Tsuda M (2009) P2Y6-evoked microglial phagocytosis. Int Rev Neurobiol 85:159–163
Koizumi S, Ohsawa K, Inoue K, Kohsaka S (2013) Purinergic receptors in microglia: functional modal shifts of microglia mediated by P2 and P1 receptors. Glia 61:47–54
Berchtold S, Ogilvie AL, Bogdan C, Mühl-Zürbes P, Ogilvie A, Schuler G, Steinkasserer A (1999) Human monocyte derived dendritic cells express functional P2X and P2Y receptors as well as ecto-nucleotidases. FEBS Lett 458:424–428
Panther E, Idzko M, Herouy Y, Rheinen H, Gebicke-Haerter PJ, Mrowietz U, Dichmann S, Norgauer J (2001) Expression and function of adenosine receptors in human dendritic cells. FASEB J 15:1963–1970
Panther E, Corinti S, Idzko M, Herouy Y, Napp M, la SA, Girolomoni G, Norgauer J (2003) Adenosine affects expression of membrane molecules, cytokine and chemokine release, and the T-cell stimulatory capacity of human dendritic cells. Blood 101:3985–3990
Challier J, Bruniquel D, Sewell AK, Laugel B (2013) Adenosine and cAMP signalling skew human dendritic cell differentiation towards a tolerogenic phenotype with defective CD8+ T-cell priming capacity. Immunology 138:402–410
Ben Addi A, Lefort A, Hua X, Libert F, Communi D, Ledent C, Macours P, Tilley SL, Boeynaems JM, Robaye B (2008) Modulation of murine dendritic cell function by adenine nucleotides and adenosine: involvement of the A2B receptor. Eur J Immunol 38:1610–1620
Novitskiy SV, Ryzhov S, Zaynagetdinov R, Goldstein AE, Huang Y, Tikhomirov OY, Blackburn MR, Biaggioni I, Carbone DP, Feoktistov I, Dikov MM (2008) Adenosine receptors in regulation of dendritic cell differentiation and function. Blood 112:1822–1831
Wilson JM, Ross WG, Agbai ON, Frazier R, Figler RA, Rieger J, Linden J, Ernst PB (2009) The A2B adenosine receptor impairs the maturation and immunogenicity of dendritic cells. J Immunol 182:4616–4623
Mascanfroni ID, Yeste A, Vieira SM, Burns EJ, Patel B, Sloma I, Wu Y, Mayo L, Ben-Hamo R, Efroni S, Kuchroo VK, Robson SC, Quintana FJ (2013) IL-27 acts on DCs to suppress the T cell response and autoimmunity by inducing expression of the immunoregulatory molecule CD39. Nat Immunol 14:1054–1063
Wilson JM, Kurtz CC, Black SG, Ross WG, Alam MS, Linden J, Ernst PB (2011) The A2B adenosine receptor promotes Th17 differentiation via stimulation of dendritic cell IL-6. J Immunol 186:6746–6752
Wei W, Du C, Lv J, Zhao G, Li Z, Wu Z, Haskó G, Xie X (2013) Blocking A2B adenosine receptor alleviates pathogenesis of experimental autoimmune encephalomyelitis via inhibition of IL-6 production and Th17 differentiation. J Immunol 190:138–146
Schnurr M, Toy T, Shin A, Hartmann G, Rothenfusser S, Soellner J, Davis ID, Cebon J, Maraskovsky E (2004) Role of adenosine receptors in regulating chemotaxis and cytokine production of plasmacytoid dendritic cells. Blood 103:1391–1397
Desrosiers MD, Cembrola KM, Fakir MJ, Stephens LA, Jama FM, Shameli A, Mehal WZ, Santamaria P, Shi Y (2007) Adenosine deamination sustains dendritic cell activation in inflammation. J Immunol 179:1884–1892
Ghaemi Oskouie F, Shameli A, Yang A, Desrosiers MD, Mucsi AD, Blackburn MR, Yang Y, Santamaria P, Shi Y (2011) High levels of adenosine deaminase on dendritic cells promote autoreactive T cell activation and diabetes in nonobese diabetic mice. J Immunol 186:6798–6806
Mizumoto N, Kumamoto T, Robson SC, Sévigny J, Matsue H, Enjyoji K, Takashima A (2002) CD39 is the dominant Langerhans cell-associated ecto-NTPDase: modulatory roles in inflammation and immune responsiveness. Nat Med 8:358–365
Idzko M, Ayata K, Müller T, Dürk T, Grimm M, Baudiss K, Vieira RP, Cicko S, Boehlke C, Zech A, Sorichter S, Pelletier J, Sévigny J, Robson SC (2013) Attenuated allergic airway inflammation in Cd39 null mice. Allergy 68:472–480
Idzko M, Panther E, Bremer HC, Windisch W, Sorichter S, Herouy Y, Elsner P, Mockenhaupt M, Girolomoni G, Norgauer J (2004) Inosine stimulates chemotaxis, Ca2+-transients and actin polymerization in immature human dendritic cells via a pertussis toxin-sensitive mechanism independent of adenosine receptors. J Cell Physiol 199:149–156
Panther E, Dürk T, Ferrari D, Di Virgilio F, Grimm M, Sorichter S, Cicko S, Herouy Y, Norgauer J, Idzko M, Müller T (2012) AMP affects intracellular Ca2+ signaling, migration, cytokine secretion and T cell priming capacity of dendritic cells. PLoS One 7:e37560
Liu QH, Bohlen H, Titzer S, Christensen O, Diehl V, Hescheler J, Fleischmann BK (1999) Expression and a role of functionally coupled P2Y receptors in human dendritic cells. FEBS Lett 445:402–408
Ferrari D, la Sala A, Chiozzi P, Morelli A, Falzoni S, Girolomoni G, Idzko M, Dichmann S, Norgauer J, Di Virgilio F (2000) The P2 purinergic receptors of human dendritic cells: identification and coupling to cytokine release. FASEB J 14:2466–2476
Idzko M, Dichmann S, Ferrari D, Di Virgilio F, la Sala A, Girolomoni G, Panther E, Norgauer J (2002) Nucleotides induce chemotaxis and actin polymerization in immature but not mature human dendritic cells via activation of pertussis toxin-sensitive P2y receptors. Blood 100:925–932
Vanderstocken G, Van de Paar E, Robaye B, Di Pietrantonio L, Bondue B, Boeynaems JM, Desmecht D, Communi D (2012) Protective role of P2Y2 receptor against lung infection induced by pneumonia virus of mice. PLoS One 7:e50385
Schnurr M, Toy T, Stoitzner P, Cameron P, Shin A, Beecroft T, Davis ID, Cebon J, Maraskovsky E (2003) ATP gradients inhibit the migratory capacity of specific human dendritic cell types: implications for P2Y11 receptor signaling. Blood 102:613–620
la Sala A, Sebastiani S, Ferrari D, Di Virgilio F, Idzko M, Norgauer J, Girolomoni G (2002) Dendritic cells exposed to extracellular adenosine triphosphate acquire the migratory properties of mature cells and show a reduced capacity to attract type 1 T lymphocytes. Blood 99:1715–1722
Horckmans M, Marcet B, Marteau F, Bulté F, Maho A, Parmentier M, Boeynaems JM, Communi D (2006) Extracellular adenine nucleotides inhibit the release of major monocyte recruiters by human monocyte-derived dendritic cells. FEBS Lett 580:747–754
Schnurr M, Then F, Galambos P, Scholz C, Siegmund B, Endres S, Eigler A (2000) Extracellular ATP and TNF-α synergize in the activation and maturation of human dendritic cells. J Immunol 165:4704–4709
Wilkin F, Duhant X, Bruyns C, Suarez-Huerta N, Boeynaems JM, Robaye B (2001) The P2Y11 receptor mediates the ATP-induced maturation of human monocyte-derived dendritic cells. J Immunol 166:7172–7177
la Sala A, Ferrari D, Corinti S, Cavani A, Di Virgilio F, Girolomoni G (2001) Extracellular ATP induces a distorted maturation of dendritic cells and inhibits their capacity to initiate Th1 responses. J Immunol 166:1611–1617
Wilkin F, Stordeur P, Goldman M, Boeynaems JM, Robaye B (2002) Extracellular adenine nucleotides modulate cytokine production by human monocyte-derived dendritic cells: dual effect on IL-12 and stimulation of IL-10. Eur J Immunol 32:2409–2417
Marteau F, Gonzalez NS, Communi D, Goldman M, Boeynaems JM, Communi D (2005) Thrombospondin-1 and indoleamine 2,3-dioxygenase are major targets of extracellular ATP in human dendritic cells. Blood 106:3860–3866
Bles N, Horckmans M, Lefort A, Libert F, Macours P, El Housni H, Marteau F, Boeynaems JM, Communi D (2007) Gene expression profiling defines ATP as a key regulator of human dendritic cell functions. J Immunol 179:3550–3558
Bles N, Di Pietrantonio L, Boeynaems JM, Communi D (2010) ATP confers tumorigenic properties to dendritic cells by inducing amphiregulin secretion. Blood 116:3219–3226
Marteau F, Communi D, Boeynaems JM, Suarez Gonzalez N (2004) Involvement of multiple P2Y receptors and signaling pathways in the action of adenine nucleotides diphosphates on human monocyte-derived dendritic cells. J Leukoc Biol 76:796–803
Ben Addi A, Cammarata D, Conley PB, Boeynaems JM, Robaye B (2010) Role of the P2Y12 receptor in the modulation of murine dendritic cell function by ADP. J Immunol 185:5900–5906
Idzko M, Panther E, Sorichter S, Herouy Y, Berod L, Geissler M, Mockenhaupt M, Elsner P, Girolomoni G, Norgauer J (2004) Characterization of the biological activities of uridine diphosphate in human dendritic cells: Influence on chemotaxis and CXCL8 release. J Cell Physiol 201:286–293
Marriott I, Inscho EW, Bost KL (1999) Extracellular uridine nucleotides initiate cytokine production by murine dendritic cells. Cell Immunol 195:147–156
Skelton L, Cooper M, Murphy M, Platt A (2003) Human immature monocyte-derived dendritic cells express the G protein-coupled receptor GPR105 (KIAA0001, P2Y14) and increase intracellular calcium in response to its agonist, uridine diphosphoglucose. J Immunol 171:1941–1949
Shin A, Toy T, Rothenfusser S, Robson N, Vorac J, Dauer M, Stuplich M, Endres S, Cebon J, Maraskovsky E, Schnurr M (2008) P2Y receptor signaling regulates phenotype and IFN-α secretion of human plasmacytoid dendritic cells. Blood 111:3062–3069
Qu Y, Ramachandra L, Mohr S, Franchi L, Harding CV, Nunez G, Dubyak GR (2009) P2X7 receptor-stimulated secretion of MHC class II-containing exosomes requires the ASC/NLRP3 inflammasome but is independent of caspase-1. J Immunol 182:5052–5062
Dubyak GR (2012) P2X7 receptor regulation of non-classical secretion from immune effector cells. Cell Microbiol 14:1697–1706
Mutini C, Falzoni S, Ferrari D, Chiozzi P, Morelli A, Baricordi OR, Collo G, Ricciardi-Castagnoli P, Di Virgilio F (1999) Mouse dendritic cells express the P2X7 purinergic receptor: characterization and possible participation in antigen presentation. J Immunol 163:1958–1965
Pizzirani C, Ferrari D, Chiozzi P, Adinolfi E, Sandonà D, Savaglio E, Di Virgilio F (2007) Stimulation of P2 receptors causes release of IL-1β-loaded microvesicles from human dendritic cells. Blood 109:3856–3864
Weber FC, Esser PR, Müller T, Ganesan J, Pellegatti P, Simon MM, Zeiser R, Idzko M, Jakob T, Martin SF (2010) Lack of the purinergic receptor P2X7 results in resistance to contact hypersensitivity. J Exp Med 207:2609–2619
Sluyter R, Wiley JS (2002) Extracellular adenosine 5'-triphosphate induces a loss of CD23 from human dendritic cells via activation of P2X7 receptors. Int Immunol 14:1415–1421
Baroni M, Pizzirani C, Pinotti M, Ferrari D, Adinolfi E, Calzavarini S, Caruso P, Bernardi F, Di Virgilio F (2007) Stimulation of P2 (P2X7) receptors in human dendritic cells induces the release of tissue factor-bearing microparticles. FASEB J 21:1926–1933
Coutinho-Silva R, Persechini PM, Bisaggio RD, Perfettini JL, Neto AC, Kanellopoulos JM, Motta-Ly I, Dautry-Varsat A, Ojcius DM (1999) P2Z/P2X7 receptor-dependent apoptosis of dendritic cells. Am J Physiol 276:C1139–C1147
Nihei OK, de Carvalho AC, Savino W, Alves LA (2000) Pharmacologic properties of P2Z/P2X7 receptor characterized in murine dendritic cells: role on the induction of apoptosis. Blood 96:996–1005
Atarashi K, Nishimura J, Shima T, Umesaki Y, Yamamoto M, Onoue M, Yagita H, Ishii N, Evans R, Honda K, Takeda K (2008) ATP drives lamina propria T(H)17 cell differentiation. Nature 455:808–812
Kusu T, Kayama H, Kinoshita M, Jeon SG, Ueda Y, Goto Y, Okumura R, Saiga H, Kurakawa T, Ikeda K, Maeda Y, Nishimura J, Arima Y, Atarashi K, Honda K, Murakami M, Kunisawa J, Kiyono H, Okumura M, Yamamoto M, Takeda K (2013) Ecto-nucleoside triphosphate diphosphohydrolase 7 controls Th17 cell responses through regulation of luminal ATP in the small intestine. J Immunol 190:774–783
Fredholm BB, Sandberg G, Ernström U (1978) Cyclic AMP in freshly prepared thymocyte suspensions. Evidence for stimulation by endogenous adenosine. Biochem Pharmacol 27:2675–2682
Marone G, Plaut M, Lichtenstein LM (1978) Characterization of a specific adenosine receptor on human lymphocytes. J Immunol 121:2153–2159
Schwartz AL, Stern RC, Polmar SH (1978) Demonstration of adenosine receptor on human lymphocytes in vitro and its possible role in the adenosine deaminase-deficient form of severe combined immunodeficiency. Clin Immunol Immunopathol 9:499–505
Fredholm BB, Sandberg G (1983) Inhibition by xanthine derivatives of adenosine receptor-stimulated cyclic adenosine 3',5'-monophosphate accumulation in rat and guinea-pig thymocytes. Br J Pharmacol 80:639–644
Fishman RF, Rubin AL, Novogrodsky A, Stenzel KH (1980) Selective suppression of blastogenesis induced by different mitogens: effect of noncyclic adenosine-containing compounds. Cell Immunol 54:129–139
Bessler H, Djaldetti M, Moroz C (1982) The regulatory role of adenosine-activated T-lymphocyte subset on the immune response in humans. I. Mitogenic response and production of mediators. Cell Immunol 73:216–229
Wolberg G, Zimmerman TP, Hiemstra K, Winston M, Chu LC (1975) Adenosine inhibition of lymphocyte-mediated cytolysis: possible role of cyclic adenosine monophosphate. Science 187:957–959
Smith GP, Shah T, Webster AD, Peters TJ (1981) Studies on the kinetic properties and subcellular localization of adenosine diphosphatase activity in human peripheral blood lymphocytes. Clin Exp Immunol 46:321–326
Cuschieri A, Mughal S, Kharbat BA (1982) Ultrastructural localization of adenosine triphosphatase activity in lymphocytes activated in vitro by phytohaemagglutinin. Histochem J 14:593–607
Dornand J, Bonnafous JC, Favero J, Gartner A, Mani JC (1984) 5'Nucleotidase and adenosine deaminase activities in human lymphocytes and lymphoblastoid cell lines. Adv Exp Med Biol 165:261–266
Pechán I, Rendeková V, Niks M, Pechánová E, Krizko J (1984) Adenosine deaminase and 5'-nucleotidase activity of T- and B-lymphocytes of human peripheral blood. Biologia (Bratislava) 39:381–386
Barankiewicz J, Dosch HM, Cohen A (1988) Extracellular nucleotide catabolism in human B and T lymphocytes. The source of adenosine production. J Biol Chem 263:7094–7098
Barankiewicz J, Ronlov G, Jimenez R, Gruber HE (1990) Selective adenosine release from human B but not T lymphoid cell line. J Biol Chem 265:15738–15743
Filippini A, Taffs RE, Agui T, Sitkovsky MV (1990) Ecto-ATPase activity in cytolytic T-lymphocyte. s Protection from the cytolytic effects of extracellular ATP. J Biol Chem 265:334–340
Langston HP, Ke Y, Gewirtz AT, Dombrowski KE, Kapp JA (2003) Secretion of IL-2 and IFN-γ, but not IL-4, by antigen-specific T cells requires extracellular ATP. J Immunol 170:2962–2970
Horenstein AL, Chillemi A, Zaccarello G, Bruzzone S, Quarona V, Zito A, Serra S, Malavasi F (2013) A CD38/CD203a/CD73 ectoenzymatic pathway independent of CD39 drives a novel adenosinergic loop in human T lymphocytes. Oncoimmunology 2:e26246
Huang S, Apasov S, Koshiba M, Sitkovsky M (1997) Role of A2a extracellular adenosine receptor-mediated signaling in adenosine-mediated inhibition of T-cell activation and expansion. Blood 90:1600–1610
Koshiba M, Kojima H, Huang S, Apasov S, Sitkovsky MV (1997) Memory of extracellular adenosine A2A purinergic receptor-mediated signaling in murine T cells. J Biol Chem 272:25881–25889
Varani K, Gessi S, Dalpiaz A, Ongini E, Borea PA (1997) Characterization of A2A adenosine receptors in human lymphocyte membranes by [3H]-SCH 58261 binding. Br J Pharmacol 122:386–392
Mirabet M, Herrera C, Cordero OJ, Mallol J, Lluis C, Franco R (1999) Expression of A2B adenosine receptors in human lymphocytes: their role in T cell activation. J Cell Sci 112:491–502
Koshiba M, Rosin DL, Hayashi N, Linden J, Sitkovsky MV (1999) Patterns of A2A extracellular adenosine receptor expression in different functional subsets of human peripheral T cells. Flow cytometry studies with anti-A2A receptor monoclonal antibodies. Mol Pharmacol 55:614–624
Gessi S, Varani K, Merighi S, Cattabriga E, Avitabile A, Gavioli R, Fortini C, Leung E, Mac LS, Borea PA (2004) Expression of A3 adenosine receptors in human lymphocytes: up-regulation in T cell activation. Mol Pharmacol 65:711–719
Takahashi HK, Iwagaki H, Hamano R, Kanke T, Liu K, Sadamori H, Yagi T, Yoshino T, Sendo T, Tanaka N, Nishibori M (2007) Effect of adenosine receptor subtypes stimulation on mixed lymphocyte reaction. Eur J Pharmacol 564:204–210
Yang A, Mucsi AD, Desrosiers MD, Chen JF, Schnermann JB, Blackburn MR, Shi Y (2010) Adenosine mediated desensitization of cAMP signaling enhances T-cell responses. Eur J Immunol 40:449–459
Armstrong JM, Chen JF, Schwarzschild MA, Apasov S, Smith PT, Caldwell C, Chen P, Figler H, Sullivan G, Fink S, Linden J, Sitkovsky M (2001) Gene dose effect reveals no Gs-coupled A2A adenosine receptor reserve in murine T-lymphocytes: studies of cells from A2A-receptor-gene-deficient mice. Biochem J 354:123–130
Lappas CM, Rieger JM, Linden J (2005) A2A adenosine receptor induction inhibits IFN-γ production in murine CD4+ T cells. J Immunol 174:1073–1080
Csóka B, Himer L, Selmeczy Z, Vizi ES, Pacher P, Ledent C, Deitch EA, Spolarics Z, Németh ZH, Haskó G (2008) Adenosine A2A receptor activation inhibits T helper 1 and T helper 2 cell development and effector function. FASEB J 22:3491–3499
Apasov SG, Chen JF, Smith PT, Schwarzschild MA, Fink JS, Sitkovsky MV (2000) Study of A2A adenosine receptor gene deficient mice reveals that adenosine analogue CGS 21680 possesses no A2A receptor-unrelated lymphotoxicity. Br J Pharmacol 131:43–50
Himer L, Csóka B, Selmeczy Z, Koscsó B, Pócza T, Pacher P, Németh ZH, Deitch EA, Vizi ES, Cronstein BN, Haskó G (2010) Adenosine A2A receptor activation protects CD4+ T lymphocytes against activation-induced cell death. FASEB J 24:2631–2640
Cekic C, Sag D, Day YJ, Linden J (2013) Extracellular adenosine regulates naive T cell development and peripheral maintenance. J Exp Med 210:2693–2706
Chimote AA, Hajdu P, Kucher V, Boiko N, Kuras Z, Szilagyi O, Yun YH, Conforti L (2013) Selective inhibition of KCa3.1 channels mediates adenosine regulation of the motility of human T cells. J Immunol 191:6273–6280
Takedachi M, Qu D, Ebisuno Y, Oohara H, Joachims ML, McGee ST, Maeda E, McEver RP, Tanaka T, Miyasaka M, Murakami S, Krahn T, Blackburn MR, Thompson LF (2008) CD73-generated adenosine restricts lymphocyte migration into draining lymph nodes. J Immunol 180:6288–6296
Ring S, Oliver SJ, Cronstein BN, Enk AH, Mahnke K (2009) CD4+CD25+ regulatory T cells suppress contact hypersensitivity reactions through a CD39, adenosine-dependent mechanism. J Allergy Clin Immunol 123:1287–1296
Antonioli L, Pacher P, Vizi ES, Haskó G (2013) CD39 and CD73 in immunity and inflammation. Trends Mol Med 19:355–367
Ernst PB, Garrison JC, Thompson LF (2010) Much ado about adenosine: adenosine synthesis and function in regulatory T cell biology. J Immunol 185:1993–1998
Whiteside TL, Mandapathil M, Schuler P (2011) The role of the adenosinergic pathway in immunosuppression mediated by human regulatory T cells (Treg). Curr Med Chem 18:5217–5223
Borsellino G, Kleinewietfeld M, Di Mitri D, Sternjak A, Diamantini A, Giometto R, Hopner S, Centonze D, Bernardi G, Dell'Acqua ML, Rossini PM, Battistini L, Rotzschke O, Falk K (2007) Expression of ectonucleotidase CD39 by Foxp3+ Treg cells: hydrolysis of extracellular ATP and immune suppression. Blood 110:1225–1232
Kobie JJ, Shah PR, Yang L, Rebhahn JA, Fowell DJ, Mosmann TR (2006) T regulatory and primed uncommitted CD4 T cells express CD73, which suppresses effector CD4 T cells by converting 5'-adenosine monophosphate to adenosine. J Immunol 177:6780–6786
Deaglio S, Dwyer KM, Gao W, Friedman D, Usheva A, Erat A, Chen JF, Enjyoji K, Linden J, Oukka M, Kuchroo VK, Strom TB, Robson SC (2007) Adenosine generation catalyzed by CD39 and CD73 expressed on regulatory T cells mediates immune suppression. J Exp Med 204:1257–1265
Mandapathil M, Hilldorfer B, Szczepanski MJ, Czystowska M, Szajnik M, Ren J, Lang S, Jackson EK, Gorelik E, Whiteside TL (2010) Generation and accumulation of immunosuppressive adenosine by human CD4 + CD25highFOXP3+ regulatory T cells. J Biol Chem 285:7176–7186
Dwyer KM, Hanidziar D, Putheti P, Hill PA, Pommey S, McRae JL, Winterhalter A, Doherty G, Deaglio S, Koulmanda M, Gao W, Robson SC, Strom TB (2010) Expression of CD39 by human peripheral blood CD4+ CD25+ T cells denotes a regulatory memory phenotype. Am J Transplant 10:2410–2420
Mandler R, Birch RE, Polmar SH, Kammer GM, Rudolph SA (1982) Abnormal adenosine-induced immunosuppression and cAMP metabolism in T lymphocytes of patients with systemic lupus erythematosus. Proc Natl Acad Sci U S A 79:7542–7546
Schultz LA, Kammer GM, Rudolph SA (1988) Characterization of the human T lymphocyte adenosine receptor: comparison of normal and systemic lupus erythematosus cells. FASEB J 2:244–250
Yang Z, Day YJ, Toufektsian MC, Ramos SI, Marshall M, Wang XQ, French BA, Linden J (2005) Infarct-sparing effect of A2A -adenosine receptor activation is due primarily to its action on lymphocytes. Circulation 111:2190–2197
Yang Z, Day YJ, Toufektsian MC, Xu Y, Ramos SI, Marshall MA, French BA, Linden J (2006) Myocardial infarct-sparing effect of adenosine A2A receptor activation is due to its action on CD4+ T lymphocytes. Circulation 114:2056–2064
Sevigny CP, Li L, Awad AS, Huang L, McDuffie M, Linden J, Lobo PI, Okusa MD (2007) Activation of adenosine 2A receptors attenuates allograft rejection and alloantigen recognition. J Immunol 178:4240–4249
Han KL, Thomas SV, Koontz SM, Changpriroa CM, Ha SK, Malech HL, Kang EM (2013) Adenosine A2A receptor agonist-mediated increase in donor-derived regulatory T cells suppresses development of graft-versus-host disease. J Immunol 190:458–468
Wang L, Fan J, Chen S, Zhang Y, Curiel TJ, Zhang B (2013) Graft-versus-host disease is enhanced by selective CD73 blockade in mice. PLoS One 8:e58397
Li N, Mu L, Wang J, Zhang J, Xie X, Kong Q, Tang W, Yao X, Liu Y, Wang L, Wang G, Wang D, Jin L, Sun B, Li H (2012) Activation of the adenosine A2A receptor attenuates experimental autoimmune myasthenia gravis severity. Eur J Immunol 42:1140–1151
Alam MS, Kurtz CC, Rowlett RM, Reuter BK, Wiznerowicz E, Das S, Linden J, Crowe SE, Ernst PB (2009) CD73 is expressed by human regulatory T helper cells and suppresses proinflammatory cytokine production and Helicobacter felis-induced gastritis in mice. J Infect Dis 199:494–504
Németh ZH, Csóka B, Wilmanski J, Xu D, Lu Q, Ledent C, Deitch EA, Pacher P, Spolarics Z, Haskó G (2006) Adenosine A2A receptor inactivation increases survival in polymicrobial sepsis. J Immunol 176:5616–5626
Häusler SF, Montalbán del Barrio I, Strohschein J, Anoop CP, Engel JB, Hönig A, Ossadnik M, Horn E, Fischer B, Krockenberger M, Heuer S, Seida AA, Junker M, Kneitz H, Kloor D, Klotz KN, Dietl J, Wischhusen J (2011) Ectonucleotidases CD39 and CD73 on OvCA cells are potent adenosine-generating enzymes responsible for adenosine receptor 2A-dependent suppression of T cell function and NK cell cytotoxicity. Cancer Immunol Immunother 60:1405–1418
Nikolova M, Carriere M, Lelievre J, Muhtarova M, Bensussan A, Lévy Y (2009) Regulatory T cells inhibit CD8 T cell proliferation in HIV-1 infection through CD39/adenosine pathway. Retrovirology 6:O20
Nikolova M, Carriere M, Jenabian MA, Limou S, Younas M, Kök A, Huë S, Seddiki N, Hulin A, Delaneau O, Schuitemaker H, Herbeck JT, Mullins JI, Muhtarova M, Bensussan A, Zagury JF, Lelievre JD, Lévy Y (2011) CD39/adenosine pathway is involved in AIDS progression. PLoS Pathog 7:e1002110
Sakowicz-Burkiewicz M, Kocbuch K, Grden M, Maciejewska I, Szutowicz A, Pawelczyk T (2012) Impact of adenosine receptors on immunoglobulin production by human peripheral blood B lymphocytes. J Physiol Pharmacol 63:661–668
Saze Z, Schuler PJ, Hong CS, Cheng D, Jackson EK, Whiteside TL (2013) Adenosine production by human B cells and B cell-mediated suppression of activated T cells. Blood 122:9–18
Wilkinson JH, Robinson JM (1974) Effect of ATP on release of intracellular enzymes from damaged cells. Nature 249:662–663
Hallak GJ, Wilkinson JH (1977) Action of adenosine phosphates on the release of intracellular lactate dehydrogenase from human and rat lymphocytes. Enzyme 22:361–369
Wolberg G, Zimmerman TP, Duncan GS, Singer KH, Elion GB (1978) Inhibition of lymphocyte-mediated cytolysis by adenosine analogs. Biochemical studies concerning mechanism of action. Biochem Pharmacol 27:1487–1495
Ikehara S, Pahwa RN, Lunzer DG, Good RA, Modak MJ (1981) Adenosine 5'-triphosphate- (ATP) mediated stimulation and suppression of DNA synthesis in lymphoid cells. I. Characterization of ATP responsive cells in mouse lymphoid organs. J Immunol 127:1834–1838
Gregory SH, Kern M (1981) Mitogenic response of T-cell subclasses to agarose-linked and to free ribonucleotides. Immunology 42:451–457
Di Virgilio F, Bronte V, Collavo D, Zanovello P (1989) Responses of mouse lymphocytes to extracellular adenosine 5'-triphosphate (ATP). Lymphocytes with cytotoxic activity are resistant to the permeabilizing effects of ATP. J Immunol 143:1955–1960
Zheng LM, Zychlinsky A, Liu CC, Ojcius DM, Young JD (1991) Extracellular ATP as a trigger for apoptosis or programmed cell death. J Cell Biol 112:279–288
Lin J, Krishnaraj R, Kemp RG (1985) Exogenous ATP enhances calcium influx in intact thymocytes. J Immunol 135:3403–3410
el-Moatassim C, Dornand J, Mani JC (1987) Extracellular ATP increases cytosolic free calcium in thymocytes and initiates the blastogenesis of the phorbol 12-myristate 13-acetate-treated medullary population. Biochim Biophys Acta 927:437–444
Ross PE, Ehring GR, Cahalan MD (1997) Dynamics of ATP-induced calcium signaling in single mouse thymocytes. J Cell Biol 138:987–998
Padeh S, Cohen A, Roifman CM (1991) ATP-induced activation of human B lymphocytes via P2-purinoceptors. J Immunol 146:1626–1632
Wiley JS, Chen R, Wiley MJ, Jamieson GP (1992) The ATP4− receptor-operated ion channel of human lymphocytes: inhibition of ion fluxes by amiloride analogs and by extracellular sodium ions. Arch Biochem Biophys 292:411–418
Wiley JS, Chen R, Jamieson GP (1993) The ATP4− receptor-operated channel (P2Z class) of human lymphocytes allows Ba2+ and ethidium+ uptake: inhibition of fluxes by suramin. Arch Biochem Biophys 305:54–60
Ferrari D, Munerati M, Melchiorri L, Hanau S, Di Virgilio F, Baricordi OR (1994) Responses to extracellular ATP of lymphoblastoid cell lines from Duchenne muscular dystrophy patients. Am J Physiol 267:C886–C892
Wiley JS, Chen JR, Snook MB, Jamieson GP (1994) The P2Z-purinoceptor of human lymphocytes: actions of nucleotide agonists and irreversible inhibition by oxidized ATP. Br J Pharmacol 112:946–950
Gargett CE, Wiley JS (1997) The isoquinoline derivative KN-62 a potent antagonist of the P2Z-receptor of human lymphocytes. Br J Pharmacol 120:1483–1490
Bretschneider F, Klapperstück M, Löhn M, Markwardt F (1995) Nonselective cationic currents elicited by extracellular ATP in human B-lymphocytes. Pflugers Arch 429:691–698
Markwardt F, Löhn M, Böhm T, Klapperstück M (1997) Purinoceptor-operated cationic channels in human B lymphocytes. J Physiol 498:143–151
Chused TM, Apasov S, Sitkovsky M (1996) Murine T lymphocytes modulate activity of an ATP-activated P2Z-type purinoceptor during differentiation. J Immunol 157:1371–1380
Baricordi OR, Ferrari D, Melchiorri L, Chiozzi P, Hanau S, Chiari E, Rubini M, Di Virgilio F (1996) An ATP-activated channel is involved in mitogenic stimulation of human T lymphocytes. Blood 87:682–690
Baricordi OR, Melchiorri L, Adinolfi E, Falzoni S, Chiozzi P, Buell G, Di Virgilio F (1999) Increased proliferation rate of lymphoid cells transfected with the P2X7 ATP receptor. J Biol Chem 274:33206–33208
Schenk U, Westendorf AM, Radaelli E, Casati A, Ferro M, Fumagalli M, Verderio C, Buer J, Scanziani E, Grassi F (2008) Purinergic control of T cell activation by ATP released through pannexin-1 hemichannels. Sci Signal 1:ra6
Tokunaga A, Tsukimoto M, Harada H, Moriyama Y, Kojima S (2010) Involvement of SLC17A9-dependent vesicular exocytosis in the mechanism of ATP release during T cell activation. J Biol Chem 285:17406–17416
Yip L, Woehrle T, Corriden R, Hirsh M, Chen Y, Inoue Y, Ferrari V, Insel PA, Junger WG (2009) Autocrine regulation of T-cell activation by ATP release and P2X7 receptors. FASEB J 23:1685–1693
Yu T, Junger WG, Yuan C, Jin A, Zhao Y, Zheng X, Zeng Y, Liu J (2010) Shockwaves increase T-cell proliferation and IL-2 expression through ATP release, P2X7 receptors, and FAK activation. Am J Physiol Cell Physiol 298:C457–C464
Junger WG (2011) Immune cell regulation by autocrine purinergic signalling. Nat Rev Immunol 11:201–212
Wang CM, Ploia C, Anselmi F, Sarukhan A, Viola A (2014) Adenosine triphosphate acts as a paracrine signaling molecule to reduce the motility of T cells. EMBO J 33:1354–1364
Jamieson GP, Snook MB, Thurlow PJ, Wiley JS (1996) Extracellular ATP causes of loss of L-selectin from human lymphocytes via occupancy of P2Z purinocepters. J Cell Physiol 166:637–642
Gu B, Bendall LJ, Wiley JS (1998) Adenosine triphosphate-induced shedding of CD23 and L-selectin (CD62L) from lymphocytes is mediated by the same receptor but different metalloproteases. Blood 92:946–951
Elliott JI, Surprenant A, Marelli-Berg FM, Cooper JC, Cassady-Cain RL, Wooding C, Linton K, Alexander DR, Higgins CF (2005) Membrane phosphatidylserine distribution as a non-apoptotic signalling mechanism in lymphocytes. Nat Cell Biol 7:808–816
Moon H, Na HY, Chong KH, Kim TJ (2006) P2X7 receptor-dependent ATP-induced shedding of CD27 in mouse lymphocytes. Immunol Lett 102:98–105
Sengstake S, Boneberg EM, Illges H (2006) CD21 and CD62L shedding are both inducible via P2X7Rs. Int Immunol 18:1171–1178
Scheuplein F, Schwarz N, Adriouch S, Krebs C, Bannas P, Rissiek B, Seman M, Haag F, Koch-Nolte F (2009) NAD+ and ATP released from injured cells induce P2X7-dependent shedding of CD62L and externalization of phosphatidylserine by murine T cells. J Immunol 182:2898–2908
Foster JG, Carter E, Kilty I, MacKenzie AB, Ward SG (2013) Mitochondrial superoxide generation enhances P2X7R-mediated loss of cell surface CD62L on naive human CD4+ T lymphocytes. J Immunol 190:1551–1559
Apasov SG, Koshiba M, Chused TM, Sitovsky MV (1997) Effects of extracellular ATP and adenosine on different thymocyte subsets. Possible role of ATP-gated channels and G protein-coupled purinergic receptor. J Immunol 158:5095–5105
Nagy PV, Fehér T, Morga S, Matkó J (2000) Apoptosis of murine thymocytes induced by extracellular ATP is dose- and cytosolic pH-dependent. Immunol Lett 72:23–30
Lépine S, Le Stunff H, Lakatos B, Sulpice JC, Giraud F (2006) ATP-induced apoptosis of thymocytes is mediated by activation of P2X7 receptor and involves de novo ceramide synthesis and mitochondria. Biochim Biophys Acta 1761:73–82
Aswad F, Dennert G (2006) P2X7 receptor expression levels determine lethal effects of a purine based danger signal in T lymphocytes. Cell Immunol 243:58–65
Tsukimoto M, Maehata M, Harada H, Ikari A, Takagi K, Degawa M (2006) P2X7 receptor-dependent cell death is modulated during murine T cell maturation and mediated by dual signaling pathways. J Immunol 177:2842–2850
Schenk U, Frascoli M, Proietti M, Geffers R, Traggiai E, Buer J, Ricordi C, Westendorf AM, Grassi F (2011) ATP inhibits the generation and function of regulatory T cells through the activation of purinergic P2X receptors. Sci Signal 4:ra12
Cappelli C, López X, Labra Y, Montoya M, Fernández R, Imarai M, Rojas JL, Miranda D, Escobar A, Acuña-Castillo C (2012) Polymyxin B increases the depletion of T regulatory cell induced by purinergic agonist. Immunobiology 217:307–315
Aswad F, Kawamura H, Dennert G (2005) High sensitivity of CD4 + CD25+ regulatory T cells to extracellular metabolites nicotinamide adenine dinucleotide and ATP: a role for P2X7 receptors. J Immunol 175:3075–3083
Seman M, Adriouch S, Scheuplein F, Krebs C, Freese D, Glowacki G, Deterre P, Haag F, Koch-Nolte F (2003) NAD-induced T cell death: ADP-ribosylation of cell surface proteins by ART2 activates the cytolytic P2X7 purinoceptor. Immunity 19:571–582
Kawamura H, Aswad F, Minagawa M, Malone K, Kaslow H, Koch-Nolte F, Schott WH, Leiter EH, Dennert G (2005) P2X7 receptor-dependent and -independent T cell death is induced by nicotinamide adenine dinucleotide. J Immunol 174:1971–1979
Adriouch S, Hubert S, Pechberty S, Koch-Nolte F, Haag F, Seman M (2007) NAD+ released during inflammation participates in T cell homeostasis by inducing ART2-mediated death of naive T cells in vivo. J Immunol 179:186–194
Hubert S, Rissiek B, Klages K, Huehn J, Sparwasser T, Haag F, Koch-Nolte F, Boyer O, Seman M, Adriouch S (2010) Extracellular NAD+ shapes the Foxp3+ regulatory T cell compartment through the ART2-P2X7 pathway. J Exp Med 207:2561–2568
Trabanelli S, Ocadlíková D, Gulinelli S, Curti A, Salvestrini V, Vieira RP, Idzko M, Di Virgilio F, Ferrari D, Lemoli RM (2012) Extracellular ATP exerts opposite effects on activated and regulatory CD4+ T cells via purinergic P2 receptor activation. J Immunol 189:1303–1310
Adinolfi E, Callegari MG, Ferrari D, Bolognesi C, Minelli M, Wieckowski MR, Pinton P, Rizzuto R, Di Virgilio F (2005) Basal activation of the P2X7 ATP receptor elevates mitochondrial calcium and potential, increases cellular ATP levels, and promotes serum-independent growth. Mol Biol Cell 16:3260–3272
Santos AA Jr, Rodrigues-Junior V, Zanin RF, Borges TJ, Bonorino C, Coutinho-Silva R, Takyia CM, Santos DS, Campos MM, Morrone FB (2013) Implication of purinergic P2X7 receptor in M. tuberculosis infection and host interaction mechanisms: a mouse model study. Immunobiology 218:1104–1112
Lang PA, Merkler D, Funkner P, Shaabani N, Meryk A, Krings C, Barthuber C, Recher M, Brück W, Häussinger D, Ohashi PS, Lang KS (2010) Oxidized ATP inhibits T-cell-mediated autoimmunity. Eur J Immunol 40:2401–2408
Chen YG, Scheuplein F, Driver JP, Hewes AA, Reifsnyder PC, Leiter EH, Serreze DV (2011) Testing the role of P2X7 receptors in the development of type 1 diabetes in nonobese diabetic mice. J Immunol 186:4278–4284
Vergani A, Fotino C, D'Addio F, Tezza S, Podetta M, Gatti F, Chin M, Bassi R, Molano RD, Corradi D, Gatti R, Ferrero ME, Secchi A, Grassi F, Ricordi C, Sayegh MH, Maffi P, Pileggi A, Fiorina P (2013) Effect of the purinergic inhibitor oxidized ATP in a model of islet allograft rejection. Diabetes 62:1665–1675
Vergani A, Tezza S, D'Addio F, Fotino C, Liu K, Niewczas M, Bassi R, Molano RD, Kleffel S, Petrelli A, Soleti A, Ammirati E, Frigerio M, Visner G, Grassi F, Ferrero ME, Corradi D, Abdi R, Ricordi C, Sayegh MH, Pileggi A, Fiorina P (2013) Long-term heart transplant survival by targeting the ionotropic purinergic receptor P2X7. Circulation 127:463–475
Heiss K, Jänner N, Mähnss B, Schumacher V, Koch-Nolte F, Haag F, Mittrücker HW (2008) High sensitivity of intestinal CD8+ T cells to nucleotides indicates P2X7 as a regulator for intestinal T cell responses. J Immunol 181:3861–3869
Wilhelm K, Ganesan J, Müller T, Dürr C, Grimm M, Beilhack A, Krempl CD, Sorichter S, Gerlach UV, Jüttner E, Zerweck A, Gärtner F, Pellegatti P, Di Virgilio F, Ferrari D, Kambham N, Fisch P, Finke J, Idzko M, Zeiser R (2010) Graft-versus-host disease is enhanced by extracellular ATP activating P2X7R. Nat Med 16:1434–1438
Chen L, Brosnan CF (2006) Exacerbation of experimental autoimmune encephalomyelitis in P2X7R−/− mice: evidence for loss of apoptotic activity in lymphocytes. J Immunol 176:3115–3126
Sharp AJ, Polak PE, Simonini V, Lin SX, Richardson JC, Bongarzone ER, Feinstein DL (2008) P2x7 deficiency suppresses development of experimental autoimmune encephalomyelitis. J Neuroinflammation 5:33
Freedman BD, Liu QH, Gaulton G, Kotlikoff MI, Hescheler J, Fleischmann BK (1999) ATP-evoked Ca2+ transients and currents in murine thymocytes: possible role for P2X receptors in death by neglect. Eur J Immunol 29:1635–1646
Woehrle T, Yip L, Elkhal A, Sumi Y, Chen Y, Yao Y, Insel PA, Junger WG (2010) Pannexin-1 hemichannel-mediated ATP release together with P2X1 and P2X4 receptors regulate T-cell activation at the immune synapse. Blood 116:3475–3484
Loomis WH, Namiki S, Ostrom RS, Insel PA, Junger WG (2003) Hypertonic stress increases T cell interleukin-2 expression through a mechanism that involves ATP release, P2 receptor, and p38 MAPK activation. J Biol Chem 278:4590–4596
Woehrle T, Yip L, Manohar M, Sumi Y, Yao Y, Chen Y, Junger WG (2010) Hypertonic stress regulates T cell function via pannexin-1 hemichannels and P2X receptors. J Leukoc Biol 88:1181–1189
Frascoli M, Marcandalli J, Schenk U, Grassi F (2012) Purinergic P2X7 receptor drives T cell lineage choice and shapes peripheral γδ cells. J Immunol 189:174–180
Manohar M, Hirsh MI, Chen Y, Woehrle T, Karande AA, Junger WG (2012) ATP release and autocrine signaling through P2X4 receptors regulate γδ T cell activation. J Leukoc Biol 92:787–794
Koshiba M, Apasov S, Sverdlov V, Chen P, Erb L, Turner JT, Weisman GA, Sitkovsky MV (1997) Transient up-regulation of P2Y2 nucleotide receptor mRNA expression is an immediate early gene response in activated thymocytes. Proc Natl Acad Sci U S A 94:831–836
Somers GR, Hammet FM, Trute L, Southey MC, Venter DJ (1998) Expression of the P2Y6 purinergic receptor in human T cells infiltrating inflammatory bowel disease. Lab Invest 78:1375–1383
Tsukimoto M, Tokunaga A, Harada H, Kojima S (2009) Blockade of murine T cell activation by antagonists of P2Y6 and P2X7 receptors. Biochem Biophys Res Commun 384:512–518
Giannattasio G, Ohta S, Boyce JR, Xing W, Balestrieri B, Boyce JA (2011) The purinergic G protein-coupled receptor 6 inhibits effector T cell activation in allergic pulmonary inflammation. J Immunol 187:1486–1495
Scrivens M, Dickenson JM (2005) Functional expression of the P2Y14 receptor in murine T-lymphocytes. Br J Pharmacol 146:435–444
Duhant X, Schandené L, Bruyns C, Gonzalez NS, Goldman M, Boeynaems JM, Communi D (2002) Extracellular adenine nucleotides inhibit the activation of human CD4+ T lymphocytes. J Immunol 169:15–21
Priebe T, Platsoucas CD, Nelson JA (1990) Adenosine receptors and modulation of natural killer cell activity by purine nucleosides. Cancer Res 50:4328–4331
Raskovalova T, Lokshin A, Huang X, Jackson EK, Gorelik E (2006) Adenosine-mediated inhibition of cytotoxic activity and cytokine production by IL-2/NKp46-activated NK cells: involvement of protein kinase A isozyme I (PKA I). Immunol Res 36:91–99
Lappas CM, Day YJ, Marshall MA, Engelhard VH, Linden J (2006) Adenosine A2A receptor activation reduces hepatic ischemia reperfusion injury by inhibiting CD1d-dependent NKT cell activation. J Exp Med 203:2639–2648
Nowak M, Lynch L, Yue S, Ohta A, Sitkovsky M, Balk SP, Exley MA (2010) The A2aR adenosine receptor controls cytokine production in iNKT cells. Eur J Immunol 40:682–687
Subramanian M, Kini R, Madasu M, Ohta A, Nowak M, Exley M, Sitkovsky M, Ohta A (2014) Extracellular adenosine controls NKT-cell-dependent hepatitis induction. Eur J Immunol 44:1119–1129
Wallace KL, Linden J (2010) Adenosine A2A receptors induced on iNKT and NK cells reduce pulmonary inflammation and injury in mice with sickle cell disease. Blood 116:5010–5020
Field JJ, Lin G, Okam MM, Majerus E, Keefer J, Onyekwere O, Ross A, Campigotto F, Neuberg D, Linden J, Nathan DG (2013) Sickle cell vaso-occlusion causes activation of iNKT cells that is decreased by the adenosine A2A receptor agonist regadenoson. Blood 121:3329–3334
Lin G, Field JJ, Yu JC, Ken R, Neuberg D, Nathan DG, Linden J (2013) NF-κB is activated in CD4+ iNKT cells by sickle cell disease and mediates rapid induction of adenosine A2A receptors. PLoS One 8:e74664
Beavis PA, Divisekera U, Paget C, Chow MT, John LB, Devaud C, Dwyer K, Stagg J, Smyth MJ, Darcy PK (2013) Blockade of A2A receptors potently suppresses the metastasis of CD73+ tumors. Proc Natl Acad Sci U S A 110:14711–14716
Harish A, Hohana G, Fishman P, Arnon O, Bar-Yehuda S (2003) A3 adenosine receptor agonist potentiates natural killer cell activity. Int J Oncol 23:1245–1249
Jeffe F, Stegmann KA, Broelsch F, Manns MP, Cornberg M, Wedemeyer H (2009) Adenosine and IFN-α synergistically increase IFN-γ production of human NK cells. J Leukoc Biol 85:452–461
Henriksson T (1983) Inhibition of natural killing by adenosine ribonucleotides. Immunol Lett 7:171–176
Schmidt A, Ortaldo JR, Herberman RB (1984) Inhibition of human natural killer cell reactivity by exogenous adenosine 5'-triphosphate. J Immunol 132:146–150
Krishnaraj R (1992) Negative modulation of human NK cell activity by purinoceptors. 1. Effect of exogenous adenosine triphosphatea. Cell Immunol 141:306–322
Krishnaraj R (1992) Negative modulation of human NK cell activity by purinoceptors. 2. Age-associated, gender-specific partial loss of sensitivity to ATP. Cell Immunol 144:11–21
Gorini S, Callegari G, Romagnoli G, Mammi C, Mavilio D, Rosano G, Fini M, Di Virgilio F, Gulinelli S, Falzoni S, Cavani A, Ferrari D, la Sala A (2010) ATP secreted by endothelial cells blocks CX3CL 1-elicited natural killer cell chemotaxis and cytotoxicity via P2Y11 receptor activation. Blood 116:4492–4500
Kawamura H, Aswad F, Minagawa M, Govindarajan S, Dennert G (2006) P2X7 receptors regulate NKT cells in autoimmune hepatitis. J Immunol 176:2152–2160
Beldi G, Wu Y, Banz Y, Nowak M, Miller L, Enjyoji K, Haschemi A, Yegutkin GG, Candinas D, Exley M, Robson SC (2008) Natural killer T cell dysfunction in CD39-null mice protects against concanavalin A-induced hepatitis. Hepatology 48:841–852
Nowak-Machen M, Schmelzle M, Hanidziar D, Junger W, Exley M, Otterbein L, Wu Y, Csizmadia E, Doherty G, Sitkovsky M, Robson SC (2013) Pulmonary natural killer T cells play an essential role in mediating hyperoxic acute lung injury. Am J Respir Cell Mol Biol 48:601–609
Di Virgilio F, Ferrari D, Chiozzi P, Falzoni S, Sanz JM, dal Susino M, Mutini C, Hanau S, Baricordi OR (1996) Purinoceptor function in the immune system. Drug Dev Res 39:319–329
Di Virgilio F, Chiozzi P, Ferrari D, Falzoni S, Sanz JM, Morelli A, Torboli M, Bolognesi G, Baricordi OR (2001) Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood 97:587–600
Di Virgilio F, Borea PA, Illes P (2001) P2 receptors meet the immune system. Trends Pharmacol Sci 22:5–7
Smith PT, Armstrong J, Koshiba M, Huang S, Apasov S, Sitkovsky M (1998) Studies of expression and possible functional role of purinergic receptors in cell-mediated immunity: Experimental approaches, controls, and caveats. Drug Dev Res 45:229–244
Burnstock G (2001) Overview of P2 receptors: possible functions in immune cells. Drug Dev Res 53:53–59
Di Virgilio F (2000) Dr. Jekyll/Mr. Hyde: the dual role of extracellular ATP. J Auton Nerv Syst 81:59–63
Di Virgilio F (2007) Purinergic signalling in the immune system. A brief update. Purinergic Signal 3:1–3
Sitkovsky MV (1998) Extracellular purines and their receptors in immunoregulation. Review of recent advances. Nihon Ika Daigaku Zasshi 65:351–357
Armstrong S, Korcok J, Sims SM, Dixon SJ (2007) Activation of transcription factors by extracellular nucleotides in immune and related cell types. Purinergic Signal 3:59–69
Myrtek D, Idzko M (2007) Chemotactic activity of extracellular nucleotideson human immune cells. Purinergic Signal 3:5–11
Di Virgilio F, Ceruti S, Bramanti P, Abbracchio MP (2009) Purinergic signalling in inflammation of the central nervous system. Trends Neurosci 32:79–87
Zeiser R, Penack O, Holler E, Idzko M (2011) Danger signals activating innate immunity in graft-versus-host disease. J Mol Med (Berl) 89:833–845
Vitiello L, Gorini S, Rosano G, la Sala A (2012) Immunoregulation through extracellular nucleotides. Blood 120:511–518
Jacob F, Novo CP, Bachert C, Crombruggen K (2013) Purinergic signaling in inflammatory cells: P2 receptor expression, functional effects, and modulation of inflammatory responses. Purinergic Signall 9:285–306
Idzko M, Ferrari D, Eltzschig HK (2014) Nucleotide signalling during inflammation. Nature 509:310–317
Kammer GM (1986) Adenosine: emerging role as an immunomodifying agent. J Lab Clin Sept:255–256
Gessi S, Varani K, Merighi S, Ongini E, Borea PA (2000) A2A adenosine receptors in human peripheral blood cells. Br J Pharmacol 129:2–11
Haskó G, Deitch EA, Szabo C, Nemeth ZH, Vizi ES (2002) Adenosine: a potential mediator of immunosuppression in multiple organ failure. Curr Opin Pharmacol 2:440–444
Haskó G, Cronstein BN (2004) Adenosine: an endogenous regulator of innate immunity. Trends Immunol 25:33–39
McCallion K, Harkin DW, Gardiner KR (2004) Role of adenosine in immunomodulation: review of the literature. Crit Care Med 32:273–277
Sitkovsky MV, Ohta A (2005) The 'danger' sensors that STOP the immune response: the A2 adenosine receptors? Trends Immunol 26:299–304
Kumar V, Sharma A (2009) Adenosine: an endogenous modulator of innate immune system with therapeutic potential. Eur J Pharmacol 616:7–15
Ohta A, Sitkovsky M (2009) The adenosinergic immunomodulatory drugs. Curr Opin Pharmacol 9:501–506
Drygiannakis I, Ernst PB, Lowe D, Glomski IJ (2011) Immunological alterations mediated by adenosine during host-microbial interactions. Immunol Res 50:69–77
Ramakers BP, Riksen NP, van der Hoeven JG, Smits P, Pickkers P (2011) Modulation of innate immunity by adenosine receptor stimulation. Shock 36:208–215
Antonioli L, Blandizzi C, Pacher P, Haskó G (2013) Immunity, inflammation and cancer: a leading role for adenosine. Nat Rev Cancer 13:842–857
Antonioli L, Csóka B, Fornai M, Colucci R, Kókai E, Blandizzi C, Haskó G (2014) Adenosine and inflammation: what's new on the horizon? Drug Discov Today 19:1051–1068
Salmi M, Jalkanen S (2005) Cell-surface enzymes in control of leukocyte trafficking. Nat Rev Immunol 5:760–771
Dwyer KM, Deaglio S, Gao W, Friedman D, Strom TB, Robson SC (2007) CD39 and control of cellular immune responses. Purinergic Signal 3:171–180
Beavis PA, Stagg J, Darcy PK, Smyth MJ (2012) CD73: a potent suppressor of antitumor immune responses. Trends Immunol 33:231–237
Junger WG (2008) Purinergic regulation of neutrophil chemotaxis. Cell Mol Life Sci 65:2528–2540
Grassi F (2010) Purinergic control of neutrophil activation. J Mol Cell Biol 2:176–177
Barletta KE, Ley K, Mehrad B (2012) Regulation of neutrophil function by adenosine. Arterioscler Thromb Vasc Biol 32:856–864
Ferrari D, la Sala A, Panther E, Norgauer J, Di Virgilio F, Idzko M (2006) Activation of human eosinophils via P2 receptors: novel findings and future perspectives. J Leukoc Biol 79:7–15
Bulanova E, Bulfone-Paus S (2010) P2 receptor-mediated signaling in mast cell biology. Purinergic Signal 6:3–17
Skaper SD, Giusti P, Facci L (2012) Microglia and mast cells: two tracks on the road to neuroinflammation. FASEB J 26:3103–3117
Weisman GA, Erb L, Garrad RC, Theiss PM, Santiago-Pérez LI, Flores RV, Santos-Berríos C, Méndez Y, González FA (1998) P2Y nucleotide receptors in the immune system: Signaling by a P2Y2 receptor in U937 monocytes. Drug Dev Res 45:222–228
Haskó G, Pacher P (2012) Regulation of macrophage function by adenosine. Arterioscler Thromb Vasc Biol 32:865–869
Inoue K (2008) Purinergic systems in microglia. Cell Mol Life Sci 65:3074–3080
Burnstock G, Verkhratsky A (2012) Purinergic signalling and the nervous system. Springer, Heidelberg/Berlin, pp 1–715
Ferrari D, Gorini S, Callegari G, la Sala A (2007) Shaping immune responses through the activation of dendritic cells' P2 receptors. Purinergic Signal 3:99–107
Salter RD, Watkins SC (2009) Dendritic cell altered states: what role for calcium? Immunol Rev 231:278–288
Kefford RF, Fox RM (1983) Purinogenic lymphocytotoxicity: clues to a wider chemotherapeutic potential for the adenosine deaminase inhibitors. Cancer Chemother Pharmacol 10:73–78
Marone G, Vigorita S, Triggiani M, Condorelli M (1986) Adenosine receptors on human lymphocytes. Adv Exp Med Biol 195:7–14
Goding JW, Howard MC (1998) Ecto-enzymes of lymphoid cells. Immunol Rev 161:5–10
Gessi S, Varani K, Merighi S, Fogli E, Sacchetto V, Benini A, Leung E, Mac-Lennan S, Borea PA (2007) Adenosine and lymphocyte regulation. Purinergic Signal 3:109–116
Leavy O (2007) Regulatory T cells: Adding adenosine to the mix. Nat Rev Immunol 7:493
Zarek PE, Powell JD (2007) Adenosine and anergy. Autoimmunity 40:425–432
Sitkovsky M, Lukashev D, Deaglio S, Dwyer K, Robson SC, Ohta A (2008) Adenosine A2A receptor antagonists: blockade of adenosinergic effects and T regulatory cells. Br J Pharmacol 153(Suppl 1):S457–S464
Linden J, Cekic C (2012) Regulation of lymphocyte function by adenosine. Arterioscler Thromb Vasc Biol 32:2097–2103
Di Virgilio F, Vishwanath V, Ferrari D (2001) On the role of the P2X7 receptor in the immune system. In: Abbracchio MP, Williams M (eds) Handbook of Experimental Pharmacology, Volume 151/II. Purinergic and Pyrimidinergic Signalling II - Cardiovascular, Respiratory, Immune, Metabolic and Gastrointestinal Tract Function. Springer-Verlag, Berlin, pp 356–374
Haag F, Adriouch S, Brass A, Jung C, Möller S, Scheuplein F, Bannas P, Seman M, Koch-Nolte F (2007) Extracellular NAD and ATP: Partners in immune cell modulation. Purinergic Signal 3:71–81
Costa-Junior HM, Marques-da-Silva C, Vieira FS, Monção-Ribeiro LC, Coutinho-Silva R (2011) Lipid metabolism modulation by the P2X7 receptor in the immune system and during the course of infection: new insights into the old view. Purinergic Signal 7:381–392
Yamada T, Chakrabarty AM (2004) ATP-utilizing enzymes, purinergic receptor modulation, cupredoxins and mammalian cell death. In: Ramos JL (ed) Pseudomonas. Kluwer Academic/Plenum Publishers, New York, pp 47–67
Coutinho-Silva R, Monteiro da Cruz C, Persechini PM, Ojcius DM (2007) The role of P2 receptors in controlling infections by intracellular pathogens. Purinergic Signal 3:83–90
Coutinho-Silva R, Corrêa G, Sater AA, Ojcius DM (2009) The P2X7 receptor and intracellular pathogens: a continuing struggle. Purinergic Signal 5:197–204
Wewers MD, Sarkar A (2009) P2X7 receptor and macrophage function. Purinergic Signal 5:189–195
Bald D, Koul A (2010) Respiratory ATP synthesis: the new generation of mycobacterial drug targets? FEMS Microbiol Lett 308:1–7
Acknowledgments
We are greatly indebted to the superb supporting work in the preparation of this manuscript by Dr. Gill Knight.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Burnstock, G., Boeynaems, JM. Purinergic signalling and immune cells. Purinergic Signalling 10, 529–564 (2014). https://doi.org/10.1007/s11302-014-9427-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-014-9427-2