Abstract
Background and Objectives
Inhibition of brain aminopeptidase A (APA), which converts angiotensin II into angiotensin III, has emerged as a novel antihypertensive treatment, as demonstrated in several experimental animal models. QGC001 (originally named RB150) is a prodrug of the specific and selective APA inhibitor EC33, and as such it is the prototype of a new class of centrally acting antihypertensive agents. Given by the oral route in hypertensive rats, it enters the brain and generates EC33, which blocks the brain renin–angiotensin system activity and normalises blood pressure. The aim of the present study was to evaluate the safety, pharmacokinetics and pharmacodynamic effects of QGC001 in humans.
Design and Methods
Fifty-six healthy male volunteers were randomly assigned to receive in double-blind and fasted conditions single oral doses of 10, 50, 125, 250, 500, 750, 1,000 and 1,250 mg of QGC001 (n = 6/dose) or placebo (n = 2/dose). We measured plasma and urine concentrations of both QGC001 and EC33 by liquid chromatography–tandem mass spectrometry, plasma renin concentrations (PRC), plasma and free urine aldosterone (PAldo and UAldo), plasma copeptine (PCop), and plasma and urine cortisol (PCort and UCort) concentrations, and supine systolic blood pressure (SBP), diastolic blood pressure (DBP) and heart rate (HR) at various time points.
Results
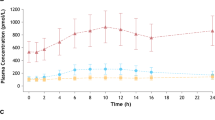
All doses of QGC001 were clinically and biologically well-tolerated. Peak plasma concentrations (C max) of QGC001 and EC33 increased linearly with the dose, with a median time to reach C max (t max) of 1.5 h for QGC001 and 3.0 h for EC33. The median plasma elimination half-life of QGC001 was 1.6 h consistently throughout doses. Urinary excretion of QGC001 and EC33 was below 2 % of the administered dose. When compared with placebo, QGC001 did not significantly change PRC, PAldo, UAldo, PCop, PCort or UCort. No significant change was observed for supine HR, SBP and DBP in any treatment group.
Conclusion
Single oral administration of QGC001 up to 1,250 mg in healthy volunteers was well-tolerated. Following oral administration, QGC001 is absorbed via the gastrointestinal tract and converted partially into its active metabolite EC33 in plasma. As in animal experiments, in normotensive subjects QGC001 had no effect on the systemic renin–angiotensin–aldosterone parameters and on PCop concentrations, a marker of vasopressin release. In normotensive subjects, a single dose of QCG001 had no effect on SBP, DBP or HR. These data support further evaluation of multiple oral doses of QGC001 in human volunteers and its clinical efficacy in hypertensive patients.




Similar content being viewed by others
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al., American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013 Jan 1;127(1):e6–e245.
Wright JW, Harding JW. Regulatory role of brain angiotensins in the control of physiological and behavioral responses. Brain Res Brain Res Rev. 1992;17(3):227–62.
Basso N, Ruiz P, Kurnjek ML, Cannata MA, Taquini AC. The brain renin-angiotensin system and the development of DOCA-salt hypertension. Clin Exp Hypertens. 1985;7(9):1259–68.
Ganten D, Hermann K, Bayer C, Unger T, Lang RE. Angiotensin synthesis in the brain and increased turnover in hypertensive rats. Science. 1983;221(4613):869–71.
Zini S, Fournie-Zaluski MC, Chauvel E, Roques BP, Corvol P, Llorens-Cortes C. Identification of metabolic pathways of brain angiotensin II and III using specific aminopeptidase inhibitors: predominant role of angiotensin III in the control of vasopressin release. Proc Natl Acad Sci USA. 1996;93(21):11968–73.
Chauvel EN, Coric P, Llorens-Cortes C, Wilk S, Roques BP, Fournie-Zaluski MC. Investigation of the active site of aminopeptidase A using a series of new thiol-containing inhibitors. J Med Chem. 1994;37(9):1339–46.
Fournie-Zaluski MC, et al. Potent and systemically active aminopeptidase N inhibitors designed from active-site investigation. J Med Chem. 1992;35(7):1259–66.
Reaux A, et al. Aminopeptidase A inhibitors as potential central antihypertensive agents. Proc Natl Acad Sci USA. 1999;96(23):13415–20.
Reaux A, Fournie-Zaluski MC, Llorens-Cortes C. Angiotensin III: a central regulator of vasopressin release and blood pressure. Trends Endocrinol Metab. 2001;12(4):157–62.
Fournie-Zaluski MC, Fassot C, Valentin B, Djordjijevic D, Reaux-Le Goazigo A, Corvol P, et al. Brain renin-angiotensin system blockade by systemically active aminopeptidase A inhibitors: a potential treatment of salt-dependent hypertension. Proc Natl Acad Sci USA. 2004;101(20):7775–80.
Rozenfeld R, Iturrioz X, Maigret B, Llorens-Cortes C. Contribution of molecular modeling and site-directed mutagenesis to the identification of two structural residues, Arg-220 and Asp-227, in aminopeptidase A. J Biol Chem. 2002;277(32):29242–52.
Fournie-Zaluski MC, Coric P, Turcaud S, Lucas E, Noble F, Maldonado R, et al. “Mixed inhibitor-prodrug” as a new approach toward systemically active inhibitors of enkephalin-degrading enzymes. J Med Chem. 1992;35(13):2473–81.
Bodineau L, Frugière A, Marc Y, Inguimbert N, Fassot C, Balavoine F, et al. Orally active aminopeptidase A inhibitors reduce blood pressure: a new strategy for treating hypertension. Hypertension. 2008;51(5):1318–25.
Marc Y, Gao J, Balavoine F, Michaud A, Roques BP, Llorens-Cortes C. Central antihypertensive effects of orally active aminopeptidase A inhibitors in spontaneously hypertensive rats. Hypertension. 2012;60(2):411–8.
Marc Y, Llorens-Cortes C. The role of the brain renin-angiotensin system in hypertension: implications for new treatment. Prog Neurobiol. 2011;95(2):89–103.
Morgenthaler NG, Struck J, Jochberger S, Dünser MW. Copeptin: clinical use of a new biomarker. Trends Endocrinol Metab. 2008;19(2):43–9.
Evans WE, Schentag JJ, Jusko WJ. Applied pharmacokinetics: principles of therapeutic drug monitoring. 3rd ed. Baltimore: Lippincott Williams & Wilkins; 1992.
Wuerzner G, Azizi M. Renin inhibition with aliskiren. Clin Exp Pharmacol Physiol. 2008;35(4):426–30.
Uchino H, Kanai Y, Kim DK, Wempe MF, Chairoungdua A, Morimoto E, et al. Transport of amino acid-related compounds mediated by L-type amino acid transporter 1 (LAT1): insights into the mechanisms of substrate recognition. Mol Pharmacol. 2002;61(4):729–37.
Azizi M, Bissery A, Bura-Riviere A, Menard J. Dual renin-angiotensin system blockade restores blood pressure-renin dependency in individuals with low renin concentrations. J Hypertens. 2003;21(10):1887–95.
Lachurié ML, Azizi M, Guyene TT, Alhenc-Gelas F, Ménard J. Angiotensin-converting enzyme gene polymorphism has no influence on the circulating renin-angiotensin-aldosterone system or blood pressure in normotensive subjects. Circulation. 1995;91(12):2933–42.
De Mota N, Iturrioz X, Claperon C, Bodineau L, Fassot C, Roques BP, et al. Human brain aminopeptidase A: biochemical properties and distribution in brain nuclei. J Neurochem. 2008;106(1):416–28.
Ma TK, Kam KK, Yan BP, Lam YY. Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. Br J Pharmacol. 2010;160(6):1273–92.
Volpe M, Pontremoli R, Borghi C. Direct renin inhibition: from pharmacological innovation to novel therapeutic opportunities. High Blood Press Cardiovasc Prev. 2011;18(3):93–105.
Acknowledgments
This study was sponsored by Quantum Genomics SA, France. The authors thank Biotrial’s staff at the Clinical Unit, in particular Dr. Pascale Koussignian and Dr. Didier Chassard for their work during the entire conduct of the study, and Bertin Pharma’s staff for the analysis of the plasma and urinary pharmacokinetic samples. The research leading to these results has received funding from the French Agence Nationale de la Recherche (BiotecS-ANR-08-BIOT-004), from the Institut National de la Santé et de la Recherche Médicale (INSERM) and Collège de France.
Conflict of interest
FB is a full-time employee of Quantum Genomics SA and holds stock options in the company. CL-C, MA, DB, NDM and BR have no conflict of interest.
Author Contributions
Fabrice Balavoine, Michel Azizi, Bernard Roques and Catherine Llorens-Cortes wrote the manuscript.
Fabrice Balavoine, Michel Azizi, Bernard Roques and Catherine Llorens-Cortes designed the research.
Fabrice Balavoine, Michel Azizi and Catherine Llorens-Cortes analysed the data.
Damien Bergerot, Nadia De Mota and Remi Patouret performed the experiments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balavoine, F., Azizi, M., Bergerot, D. et al. Randomised, Double-Blind, Placebo-Controlled, Dose-Escalating Phase I Study of QGC001, a Centrally Acting Aminopeptidase A Inhibitor Prodrug. Clin Pharmacokinet 53, 385–395 (2014). https://doi.org/10.1007/s40262-013-0125-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-013-0125-y